Background One windy morning, as Paul Marquez pulled into the parking lot of Sierra Veterans Affairs Medical
Question:
Background
One windy morning, as Paul Marquez pulled into the parking lot of Sierra Veterans Affairs Medical Center (SVAMC), he was struck by the sound of the American flag flapping overhead. As he entered the double doors to the facility, his eyes fixated on the brass plaque that hung in the hallway. The plaque bears the mission of the Department of Veterans Affairs (VA): “To care for him who shall have borne the battle and for his widow and his orphan.”
That day, more than any other, Mr. Marquez found himself deep in thought. He chose to work at the VA because of its worthy mission, but now he was unsure how to best carry out this mission in light of his current predicament.
Mr. Marquez was assistant chief of the Human Resource and Management Service (HRMS) department at SVAMC. The year before, in 1996, he was charged with overseeing the strategic reduction of the facility’s workforce— a move ordered by SVAMC’s executive leadership team (ELT) in response to budget constraints. That morning, Mr. Marquez was due to meet with the ELT to discuss the final stages of the reduction in force (RIF).
Located in a mid-sized metropolitan area, SVAMC operates 215 beds and employs between 1,300 and 1,400 personnel. A major referral medical center, SVAMC serves the community in conjunction with the VA’s nursing home care units and its Community-Based Outpatient Clinics. Also, the medical center is affiliated with the medical, pharmacy, and nursing schools in the area.
The RIF Order
Mr. Marquez received the RIF order memo from the medical center director of SVAMC. The RIF had been approved by VA headquarters in Washington, DC, and was cleared by the director of the Veterans Integrated Service Network (VISN) for the region. The memo laid out the following reasons for the RIF:
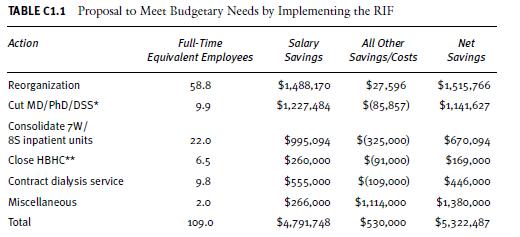
1. The need to redistribute resources in the VISN in conjunction with the strategic plan to close certain inpatient services that will enable the enhancement of outpatient services 2. An anticipated non-growth budget from the federal government that would result in an actual reduction in purchasing power of approximately 6 percent over two years 3. The need to address issues related to supervisor–employee ratios, reorganize internal functions in a more efficient manner, and abolish positions in excess of VA’s needs and/or contrary to its mission SVAMC was experiencing a shrinking reserve. In fiscal year (FY) 1995, the amount of this reserve was $4.5 million, but in FY 1996 it was down to less than $200,000. Because of this, a $7 million shortfall was predicted over the next two years and no additional funds were expected to be allocated from the VISN. Table C1.1 lays out the action plan for the RIF, a proposal expected to create a savings of more than $5 million by 1997.
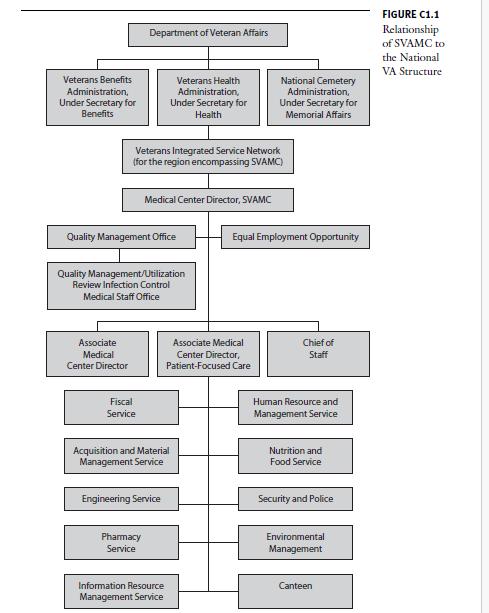
The RIF order at SVAMC came at a time of widespread transformation of the Veterans Health Administration (VHA) as a whole. (See the organizational chart in Figure C1.1 to understand how SVAMC fits into the national structure of the VA.) From 1994 through 1999, the VHA was led by visionary Under Secretary for Health Dr. Kenneth Kizer. Dr. Kizer decentralized the VHA into VISNs, giving local-level control to network directors and individual medical center leaders. Also, at this time the VA faced fiscal constraints as the government worked to balance the federal budget. Because the VA budget
is subject to the annual appropriations process conducted by Congress, it was vulnerable to fluctuations from year to year.
As with healthcare systems in other sectors, the VHA was undergoing a shift from inpatient to outpatient care. From a personnel standpoint, this shift eliminated many inpatient clinical positions. In addition, during this time a document referred to as the Farsetta Report was released, which evaluated inefficiencies within the VA system. This report catalyzed the systemwide elimination of all assistant chief positions in the VA, which made it possible for the agency to provide a greater number of health services at lower cost..........
Discussion Questions
1. In evaluating the series of events that unfolded during the RIF process, do you think the RIF was successful? Why or why not?
2. Would you have chosen a RIF as the best way to solve SVAMC’s impending budget problems? In hindsight, what alternative courses of action could have been pursued?
3. Assuming he had no other choice than to follow the directive to carry out the RIF, what additional steps could Mr.
Marquez have taken to lessen the impact of the RIF on employees? What actions can SVAMC leadership undertake now to heal the wounds caused by the RIF?
4. What are the advantages and disadvantages of using the RIF Runner software to identify employees to be targeted for the RIF?
5. From a personnel standpoint, what repercussions may arise at SVAMC as a result of the layoffs?
Step by Step Answer:

Human Resources In Healthcare Managing For Success
ISBN: 9781567932997
3rd Edition
Authors: Bruce Fried, Myron D. Fottler