Question: 1. Why are coding guidelines used? 2. What type of facility is a hospital? List the hospital categories. 3. List the components fir inpatient
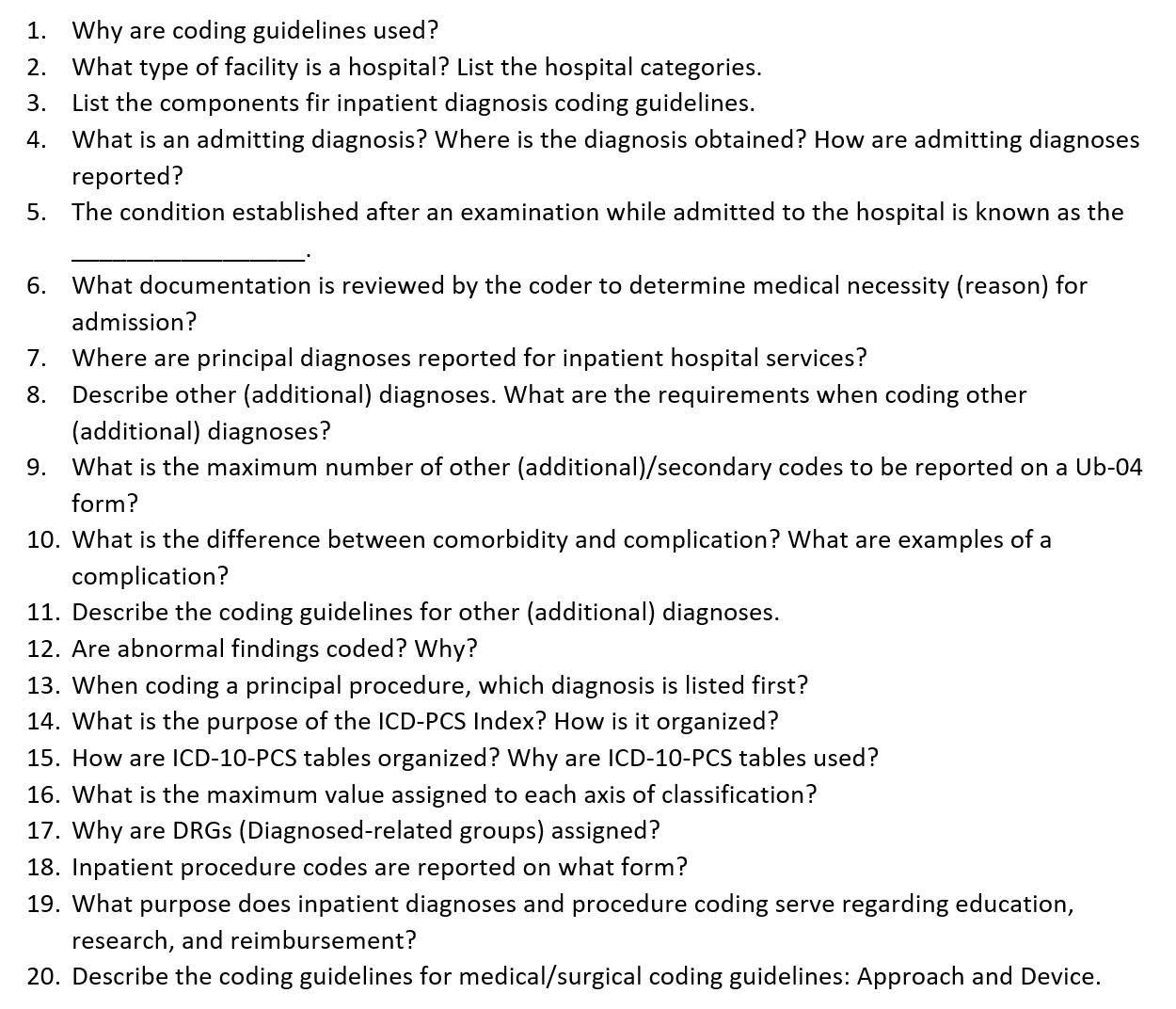
1. Why are coding guidelines used? 2. What type of facility is a hospital? List the hospital categories. 3. List the components fir inpatient diagnosis coding guidelines. 4. What is an admitting diagnosis? Where is the diagnosis obtained? How are admitting diagnoses reported? 5. The condition established after an examination while admitted to the hospital is known as the 6. What documentation is reviewed by the coder to determine medical necessity (reason) for admission? 7. Where are principal diagnoses reported for inpatient hospital services? 8. Describe other (additional) diagnoses. What are the requirements when coding other (additional) diagnoses? 9. What is the maximum number of other (additional)/secondary codes to be reported on a Ub-04 form? 10. What is the difference between comorbidity and complication? What are examples of a complication? 11. Describe the coding guidelines for other (additional) diagnoses. 12. Are abnormal findings coded? Why? 13. When coding a principal procedure, which diagnosis is listed first? 14. What is the purpose of the ICD-PCS Index? How is it organized? 15. How are ICD-10-PCS tables organized? Why are ICD-10-PCS tables used? 16. What is the maximum value assigned to each axis of classification? 17. Why are DRGs (Diagnosed-related groups) assigned? 18. Inpatient procedure codes are reported on what form? 19. What purpose does inpatient diagnoses and procedure coding serve regarding education, research, and reimbursement? 20. Describe the coding guidelines for medical/surgical coding guidelines: Approach and Device.
Step by Step Solution
There are 3 Steps involved in it
1 Why are coding guidelines used Coding guidelines are used to ensure consistency accuracy and stand... View full answer

Get step-by-step solutions from verified subject matter experts


