Question: 1. What is the mostly likely diagnosis? Why?2. Demonstrates your understanding about the pathophysiology in regard to the most likely diagnosis.3. What are the next
1. What is the mostly likely diagnosis? Why?2. Demonstrates your understanding about the pathophysiology in regard to the most likely diagnosis.3. What are the next appropriate steps in management?4. What are the appropriate patient education topic for this case?5. If not managed properly what is/are the medical/legal concern(s) may arise?
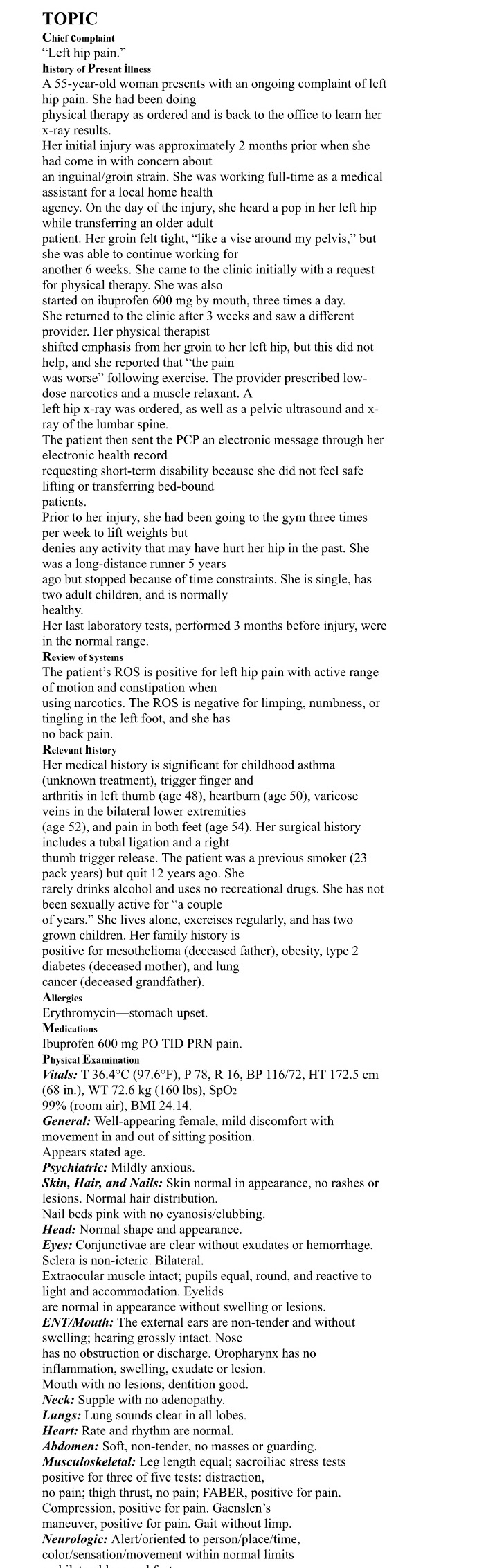
TOPIC Chicf Complaint \"Left hip pain.\" history of Present illness A 55-year-old woman presents with an ongoing complaint of left hip pain. She had been doing physical therapy as ordered and is back to the office to learn her x-ray results. Her initial injury was approximately 2 months prior when she had come 1n with concern about an inguinal/groin strain. She was working full-time as a medical assistant for a local home health agency. On the day of the injury. she heard a pop in her left hip while transferring an older adult patient. Her groin felt tight, \"like a vise around my pelvis,\" but she was able to continue working for another 6 weeks. She came to the clinic initially with a request for physical therapy. She was also started on ibuprofen 600 mg by mouth, three times a day. She returned to the clinic after 3 wecks and saw a different provider. Her physical therapist shifted emphasis from her groin to her left hip, but this did not clp, and she reported that \"the pain was worse\" following exercise. The provider prescribed low- dose narcotics and a muscle relaxant. A eft hip x-ray was ordered, as well as a pelvic ultrasound and x- ray of the lumbar spine. The patient then sent the PCP an electronic message through her electronic health record requesting short-term disability because she did not feel safe ifting or transferring bed-bound patients. Prior to her injury, she had been going to the gym three times per week to lift weights but denies any activity that may have hurt her hip in the past. She was a long-distance runner 5 years ago but stopped because of time constraints. She is single, has two adult children, and is normally calthy. Her last laboratory tests, performed 3 months before injury, were in the normal range. Review of Systems The patient's ROS is positive for lefl hip pain with active range of motion and constipation when using narcotics. The ROS is negative for limping, numbness, or tingling in the lefi foot, and she has no back pain. Relevant history Her medical history is significant for childhood asthma (unknown treatment), trigger finger and arthritis in left thumb (age 48), heartburn (age 50), varicose veins in the bilateral lower extremities (age 52), and pain in both feet (age 54). Her surgical history includes a tubal ligation and a right thumb trigger release. The patient was a previous smoker (23 pack years) but quit 12 years ago. She rarely drinks alcohol and uses no recreational drugs. She has not been sexually active for \"\"a couple of years.\" She lives alone, exercises regularly, and has two grown children. Her family history is positive for mesothelioma (deceased father), obesity, type 2 diabetes (deceased mother), and lung cancer (deceased grandfather). Allergies Erythromycinstomach upset. Medications Ibuprofen 600 mg PO TID PRN pain. Physical Examination Vitals: T 36.4C (97.6F), P78, R 16, BP 116/72, HT 172.5 cm (68 in.), WT 72.6 kg (160 Ibs), SpO: 99% (room air), BMI 24.14. General: Well-appearing female, mild discomfort with movement in and out of sitting position. Appears stated age. Psychiatric: Mildly anxious. Skin, Hair, and Nails: Skin normal in appearance, no rashes or lesions. Normal hair distribution. Nail beds pink with no cyanosis/clubbing. Head: Normal shape and appearance. Eyes: Conjunctivae are clear without exudates or hemorrhage. Sclera is non-icteric. Bilateral. Extraocular muscle intact; pupils equal, round, and reactive to light and accommodation. Eyelids are normal in appearance without swelling or lesions. ENT/Mouth: The external ears are non-tender and without swelling; hearing grossly intact. Nose has no obstruction or discharge. Oropharynx has no inflammation, swelling, exudate or lesion. Mouth with no lesions; dentition good. Neck: Supple with no adenopathy. Lungs: Lung sounds clear in all lobes. Heart: Rate and rhythm are normal. Abdomen: Soft, non-tender, no masses or guarding. Musculoskeletal: Leg length equal; sacroiliac stress tests positive for three of five tests: distraction, no pain; thigh thrust, no pain; FABER, positive for pain. Compression, positive for pain. Gaenslen's maneuver, positive for pain. Gait without limp. Neurologic: Alert/oriented to person/place/time, color/sensation/movement within normal limits