Question: How long do plans that use the C - SNP pre - enrollment verification process have to verify the qualifying chronic condition until they must
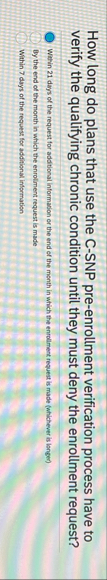
How long do plans that use the CSNP preenrollment verification process have to verify the qualifying chronic condition until they must deny the enrollment request?
Within days of the request for additional information or the end of the month in which the enrollment request is made whichever is longer
By the end of the month in which the enroliment request is made
Within days of the request for additional information
Step by Step Solution
There are 3 Steps involved in it
1 Expert Approved Answer
Step: 1 Unlock


Question Has Been Solved by an Expert!
Get step-by-step solutions from verified subject matter experts
Step: 2 Unlock
Step: 3 Unlock


