Question: please for Q1 hand-draw to be clear... The case study from the discussion for Q2: Customers drop off their prescriptions either in the drive-through counter
The case study from the discussion for Q2:
Customers drop off their prescriptions either in the drive-through counter or in the front counter of the pharmacy. Customers can request that their prescription be filled immediately. In this case, they have to wait between 15 minutes and one hour depending on the current workload. Most customers are not willing to wait that long, so they opt to nominate a pick-up time at a later point during the day. Generally, customers drop their prescriptions in the morning before going to work (or at lunchtime) and they come back to pick up the drugs after work, typically between 5pm and 6pm. When dropping their prescription, a technician asks the customer for the pick-up time and puts the prescription in a box labelled with the hour preceding the pick-up time. For example, if the customer asks to have the prescription be ready at 5pm, the technician will drop it in the box with the label 4pm (there is one box for each hour of the day).
Every hour, one of the pharmacy technicians picks up the prescriptions due to be filled in the current hour. The technician then enters the details of each prescription (e.g. doctor details, patient details and medication details) into the pharmacy system. As soon as the details of a prescription are entered, the pharmacy system performs an automated check called Drug Utilization Review (DUR). This check is meant to determine if the prescription contains any drugs that may be incompatible with other drugs that had been dispensed to the same customer in the past, or drugs that may be inappropriate for the customer taking into account the customer data maintained in the system (e.g. age).
Any alarms raised during the automated DUR are reviewed by a pharmacist who performs a more thorough check. In some cases, the pharmacist even has to call the doctor who issued the prescription in order to confirm it.
After the DUR, the system performs an insurance check in order to determine whether the customers insurance policy will pay for part or for the whole cost of the drugs. In most cases, the output of this check is that the insurance company would pay for a certain percentage of the costs, while the customer has to pay for the remaining part (also called the co-payment). The rules for determining how much the insurance company will pay and how much the customer has to pay are very complicated. Every insurance company has different rules. In some cases, the insurance policy does not cover one or several drugs in a prescription, but the drug in question can be replaced by another drug that is covered by the insurance policy. When such cases are detected, the pharmacist generally calls the doctor and/or the patient to determine if it is possible to perform the drug replacement.
Once the prescription passes the insurance check, it is assigned to a technician who collects the drugs from the shelves and puts them in a bag with the prescription stapled to it. After the technician has filled a given prescription, the bag is passed to the pharmacist who double-checks that the prescription has been filled correctly. After this quality check, the pharmacist seals the bag and puts it in the pick-up area. When a customer arrives to pick up a prescription, a technician retrieves the prescription and asks the customer for payment in case the drugs in the prescription are not (fully) covered by the customers insurance.
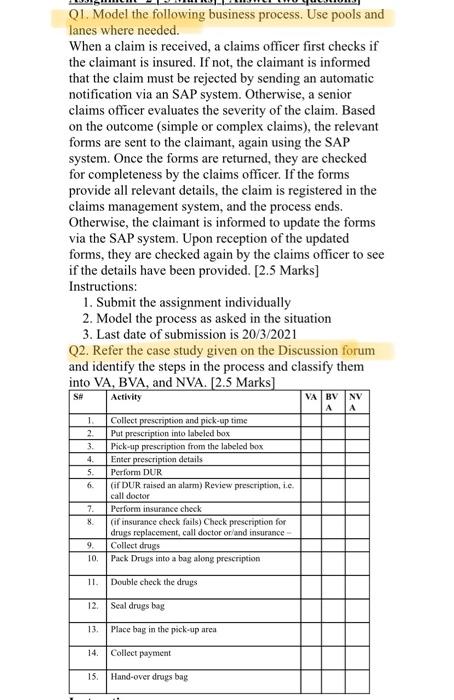
Q1. Model the following business process. Use pools and lanes where needed. When a claim is received, a claims officer first checks if the claimant is insured. If not, the claimant is informed that the claim must be rejected by sending an automatic notification via an SAP system. Otherwise, a senior claims officer evaluates the severity of the claim. Based on the outcome (simple or complex claims), the relevant forms are sent to the claimant, again using the SAP system. Once the forms are returned, they are checked for completeness by the claims officer. If the forms provide all relevant details, the claim is registered in the claims management system, and the process ends. Otherwise, the claimant is informed to update the forms via the SAP system. Upon reception of the updated forms, they are checked again by the claims officer to see if the details have been provided. [2.5 Marks] Instructions: 1. Submit the assignment individually 2. Model the process as asked in the situation 3. Last date of submission is 20/3/2021 Q2. Refer the case study given on the Discussion forum and identify the steps in the process and classify them into VA, BVA, and NVA. [2.5 Marks] VA BV NV S# Activity A 1 2 3. 4. 5. 6. Collect prescription and pick-up time Put prescription into labeled box Pick-up prescription from the labeled box Enter prescription details Perform DUR (if DUR raised an alarm) Review prescription, 1.c. call doctor Perform insurance check (if insurance check fails) Check prescription for drugs replacement, call doctor or/and insurance - Collect drugs Pack Drugs into a bag along prescription 7. 8. 9. 10. 11. Double check the drugs 12 Seal drugs bag 13 Place bag in the pick-up area 14. Collect payment 15. Hand-over drugs bag Q1. Model the following business process. Use pools and lanes where needed. When a claim is received, a claims officer first checks if the claimant is insured. If not, the claimant is informed that the claim must be rejected by sending an automatic notification via an SAP system. Otherwise, a senior claims officer evaluates the severity of the claim. Based on the outcome (simple or complex claims), the relevant forms are sent to the claimant, again using the SAP system. Once the forms are returned, they are checked for completeness by the claims officer. If the forms provide all relevant details, the claim is registered in the claims management system, and the process ends. Otherwise, the claimant is informed to update the forms via the SAP system. Upon reception of the updated forms, they are checked again by the claims officer to see if the details have been provided. [2.5 Marks] Instructions: 1. Submit the assignment individually 2. Model the process as asked in the situation 3. Last date of submission is 20/3/2021 Q2. Refer the case study given on the Discussion forum and identify the steps in the process and classify them into VA, BVA, and NVA. [2.5 Marks] VA BV NV S# Activity A 1 2 3. 4. 5. 6. Collect prescription and pick-up time Put prescription into labeled box Pick-up prescription from the labeled box Enter prescription details Perform DUR (if DUR raised an alarm) Review prescription, 1.c. call doctor Perform insurance check (if insurance check fails) Check prescription for drugs replacement, call doctor or/and insurance - Collect drugs Pack Drugs into a bag along prescription 7. 8. 9. 10. 11. Double check the drugs 12 Seal drugs bag 13 Place bag in the pick-up area 14. Collect payment 15. Hand-over drugs bag
Step by Step Solution
There are 3 Steps involved in it

Get step-by-step solutions from verified subject matter experts


