Question: Question # 2 is below Managing the Patient Experience case: Consider the pros and cons of internal and external recruitment. How might Mr. Jackson's prior
Question # 2 is below
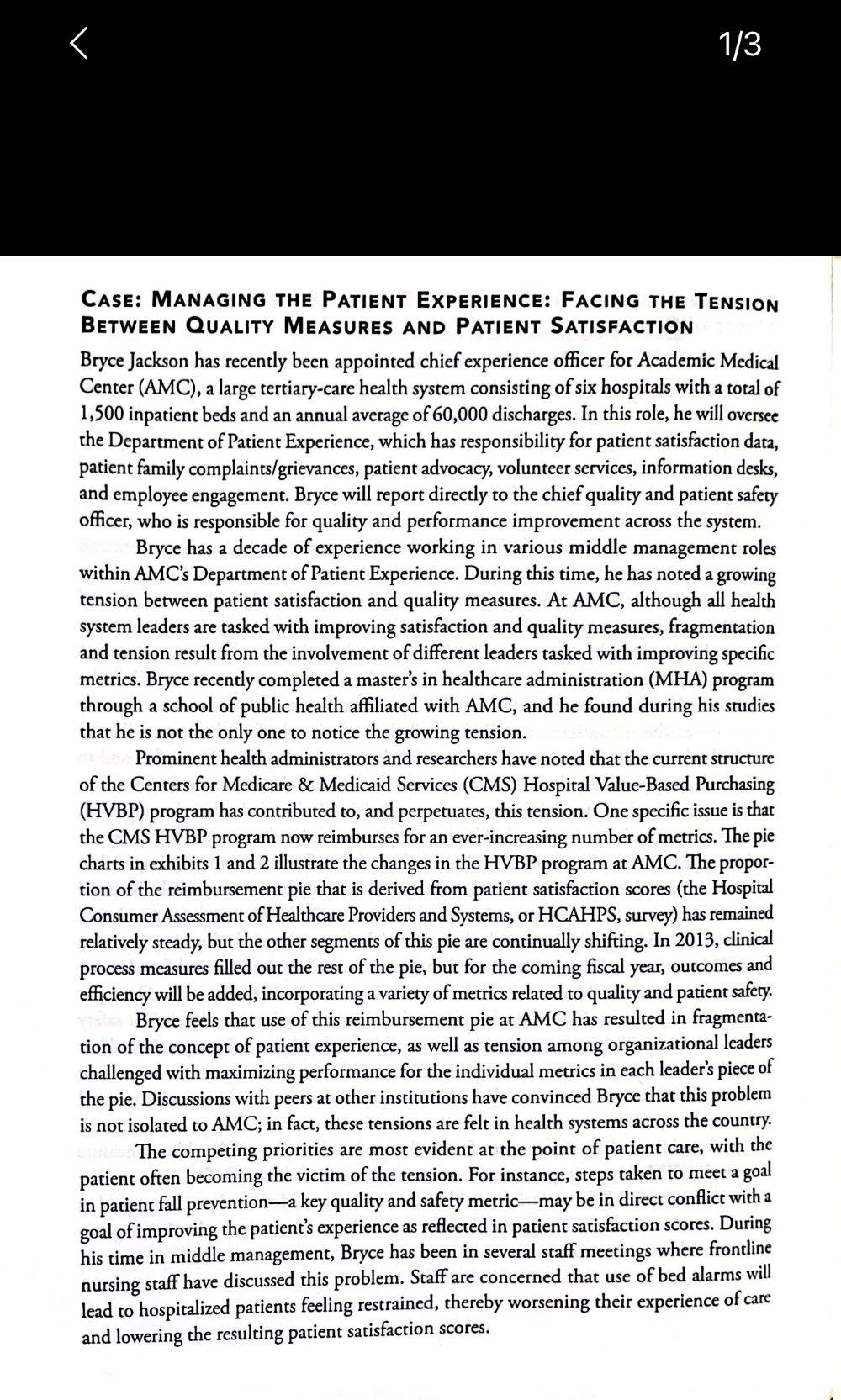
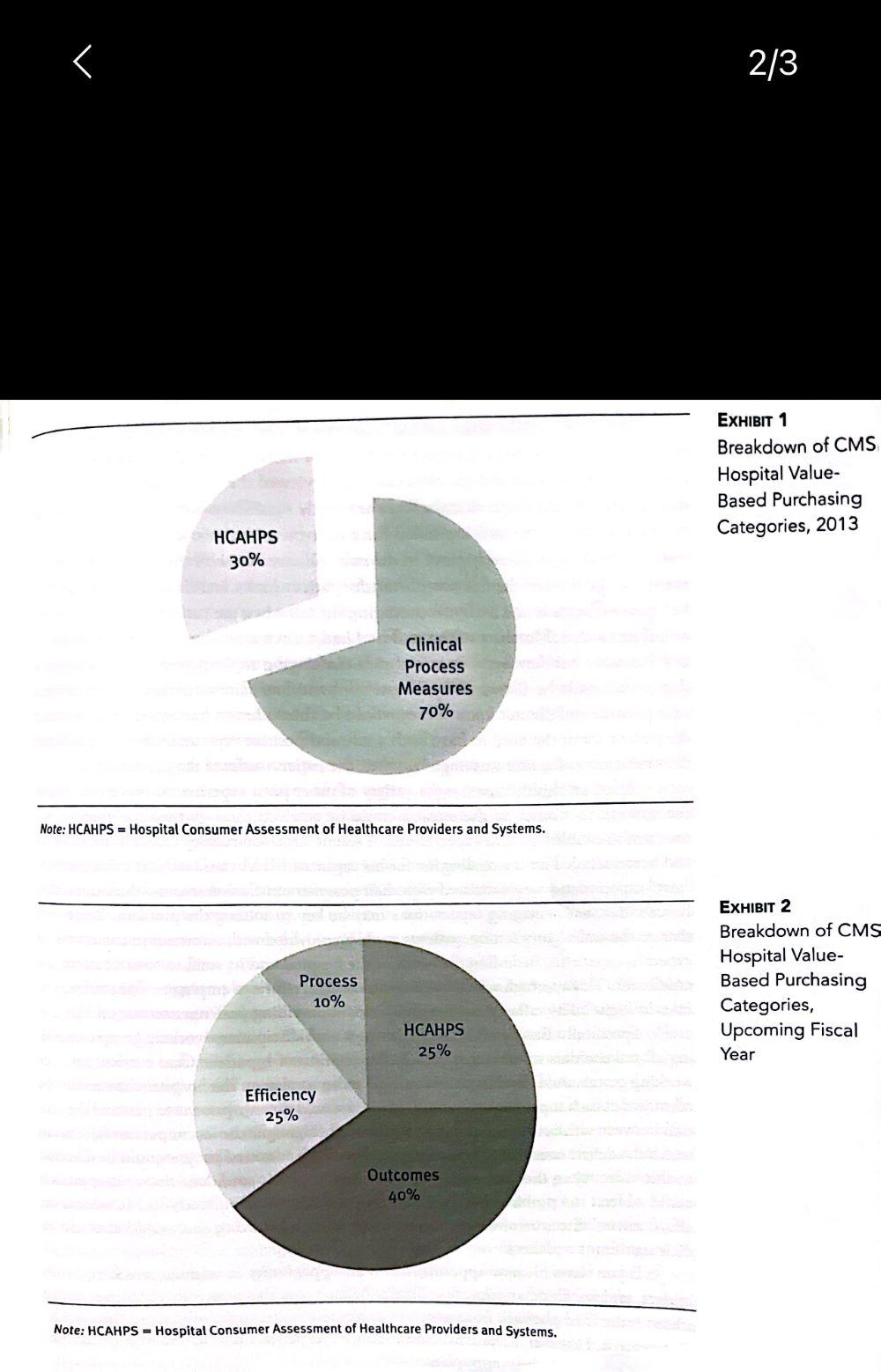
Managing the Patient Experience case: Consider the pros and cons of internal and external recruitment. How might Mr. Jackson's prior jobs and work experience affect his success as chief experience officer at Academic Medical Center? CASE: IVANAGING THE PATIENT EXPERIENCE: FACING THE TENSION BEtWEen QuALITY MEASURES AND PATIENT SATISFACTION Bryce Jackson has recently been appointed chief experience officer for Academic Medical Center (AMC), a large tertiary-care health system consisting of six hospitals with a total of 1,500 inpatient beds and an annual average of 60,000 discharges. In this role, he will oversee the Department of Patient Experience, which has responsibility for patient satisfaction data, patient family complaints/grievances, patient advocacy, volunteer services, information desks, and employee engagement. Bryce will report directly to the chief quality and patient safety officer, who is responsible for quality and performance improvement across the system. Bryce has a decade of experience working in various middle management roles within AMC's Department of Patient Experience. During this time, he has noted a growing tension between patient satisfaction and quality measures. At AMC, although all health system leaders are tasked with improving satisfaction and quality measures, fragmentation and tension result from the involvement of different leaders tasked with improving specific metrics. Bryce recently completed a master's in healthcare administration (MHA) program through a school of public health affiliated with AMC, and he found during his studies that he is not the only one to notice the growing tension. Prominent health administrators and researchers have noted that the current structure of the Centers for Medicare \& Medicaid Services (CMS) Hospital Value-Based Purchasing (HVBP) program has contributed to, and perpetuates, this tension. One specific issue is that the CMS HVBP program now reimburses for an ever-increasing number of metrics. The pie charts in exhibits 1 and 2 illustrate the changes in the HVBP program at AMC. The proportion of the reimbursement pie that is derived from patient satisfaction scores (the Hospital Consumer Assessment of Healthcare Providers and Systems, or HCAHPS, survey) has remained relatively steady, but the other segments of this pie are continually shifting. In 2013, clinical process measures filled out the rest of the pie, but for the coming fiscal year, outcomes and efficiency will be added, incorporating a variety of metrics related to quality and patient safery. Bryce feels that use of this reimbursement pie at AMC has resulted in fragmentation of the concept of patient experience, as well as tension among organizational leaders challenged with maximizing performance for the individual metrics in each leader's piece of the pie. Discussions with peers at other institutions have convinced Bryce that this problem is not isolated to AMC; in fact, these tensions are felt in health systems across the country. The competing priorities are most evident at the point of patient care, with the patient often becoming the victim of the tension. For instance, steps taken to meet a goal in patient fall prevention - a key quality and safety metric - may be in direct conflict with a goal of improving the patient's experience as reflected in patient satisfaction scores. During his time in middle management, Bryce has been in several staff meetings where frontline nursing staff have discussed this problem. Staff are concerned that use of bed alarms will lead to hospitalized patients feeling restrained, thereby worsening their experience of care and lowering the resulting patient satisfaction scores. Ex 1 Breakdown of CMS Hospital Value- Based Purchasing Categories, 2013 Note: HCAHPS = Hospital Consumer Assessment of Healthcare Providers and Systems. ExHIBIT 2 Breakdown of CMS Hospital Value- Based Purchasing Categories, Upcoming Fiscal Year Note: HCAHPS = Hospital Consumer Assessment of Healthcare Providers and Systems. Just a few months ago, a patient had been injured in a fall, triggering a patient safety event review process that highlighted this type of tension. After the fall was reported, the nurses on the care team and the physician lead reviewed the incident, and because the case was of high severity, it was discussed at the weekly significant event meeting. The administration present at the meeting called for a root-cause analysis, which took 45 days and involved speaking with every party in the case. Discussions with the nurse assigned to the patient at the time of the fall noted that the patient had a bed alarm and that the alarm had gone off twice in the 24 hours preceding the fall when the patient had tried to get out of bed unassisted. Members of the staff had had a discussion about placing the patient in arm restraints, but they were concerned about infringing on the patient's rights. They knew the patient would be distraught by the use of physical restraints, but they were under great time pressure and did not know if they would be able to have a prolonged discussion with the patient about the need to have both a safe and positive experience. Staff debate about the next course of action was ongoing when the patient suffered the injury fall. Based on this incident, and a variety of other prior experiences, Bryce has formed the opinion that much of the tension could be resolved through the development of a program to establish patient expectations. A recent large-scale survey research study, which had been included on the reading list for his capstone MHA class, indicated that patients' "met" expectations were associated with their postvisit satisfaction scores-thus supporting Bryce's idea that managing expectations may be key to solving the problem. Bryce feels that, in the ambulatory setting, patients could be provided with information about what to expect as inpatients, including the needs of the hospital and its staff, to balance safety and satisfaction. This approach would be similar to airlines' efforts to emphasize flight attendants' roles in flight safety rather than just their roles in providing passenger service on board. Specifically, Bryce envisions appointing a multidisciplinary working group comprising all stakeholders to develop a Patient Expectation of Inpatient Care curriculum. The working group could develop an educational video to play on the hospital channel on the television in each inpatient bedroom. The video would directly present to patients the tension between satisfaction and safety and specifically highlight the recent patient fall case in which the debate over arm restraints was a factor. Each admitted patient could be directed to this video when they were assigned to a room. Bryce is confident that this approach could address the problem without involving the staff nurses directly in the education effort; nurses' direct involvement could be viewed as self-serving and would also add to their significant workload. Bryce views his new appointment as an opportunity to address tensions, build bridges, and knock down silos. Specifically, he feels that this new role, chief experience officer, is the ideal platform from which to implement his program of patient expectation management. However, despite his enthusiasm, Bryce realizes that he must prioritize his agenda and develop a long-term plan. Increasing the Focus on Patient Safety at First Medical Center case: How could job design, job analysis, and job descriptions support the focus on patient safety at First Medical Center? Case: InCreasing the Focus on Patient Safety at First MediCAL CENTER At First Medical Center (FMC), the goal for the past decade has been to simultaneously improve quality and patient safety by implementing projects, initiatives, and programs either focused on an organizationwide intervention or targeted at one department, unit, or floor within the organization. This effort has resulted in a piecemeal approach to quality improvement, with one intervention layered on top of another. FMC's newly appointed chief quality and patient safety officer, Dr. Emily Frame, believes they can do better. Emily sees a major opportunity to centralize and standardize quality initiatives through a systemwide initiative focused on both cultural change and quality improvement. Specifically, she wants to implement the Crew Resource Management (CRM) program across all units of FMC. CRM is a systematic approach to training leadership, staff, and physicians, and it incorporates customizable safety tools aimed at generating permanent culture change around patient safety. Emily is aware that adopting a unified approach to safety and quality improvement will require significant organizational change, but she believes the long-term results will justify the expected difficulty. Given the circumstances at FMC, Emily believes that the first challenge will be to get the leaders of the institution to understand that a gap exists in patient safety and to recognize the opportunity for improvement. She is well aware that cultural transformation needs engaged leadership, and she knows that only through shared vision and purpose can such widespread programs succeed. If leaders are not engaged and supportive, the program will struggle to get off the ground, making the desired transformation virtually impossible. Another major challenge related to executive leadership buy-in involves the financial resources necessary for implementation. Healthcare organizations have a large number of competing financial priorities, not the least of which are training and education. Training for CRM requires dedicated time away from patient care (between two and four hours), so the organization will have to backfill that nursing and physician care time. Once put into practice, however, CRM has the potential to save money by averting patient safety events. The research literature provides some evidence for these savings, particularly in critical care and surgery specialties, though systemwide implementation has never been studied. CRM has to be seen as value added and a top priority for the organization and the care of its patients. An additional area of concern for Emily involves how she will be able to measure success. If CRM aims to improve teamwork and promote a culture of safery, how can one prove that it works? What metrics would FMC leaders, providers, and patients regard as indicators of success? As Emily well knows, cultural transformation is hard enough to define, let alone measure
Step by Step Solution
There are 3 Steps involved in it

Get step-by-step solutions from verified subject matter experts


