Question: Question 7-15 please write it CASE STUDY 7 Interorganizational Is - The National Programme for IT in the NHS Experience The National Health Service (NHS)
Question 7-15 please write it
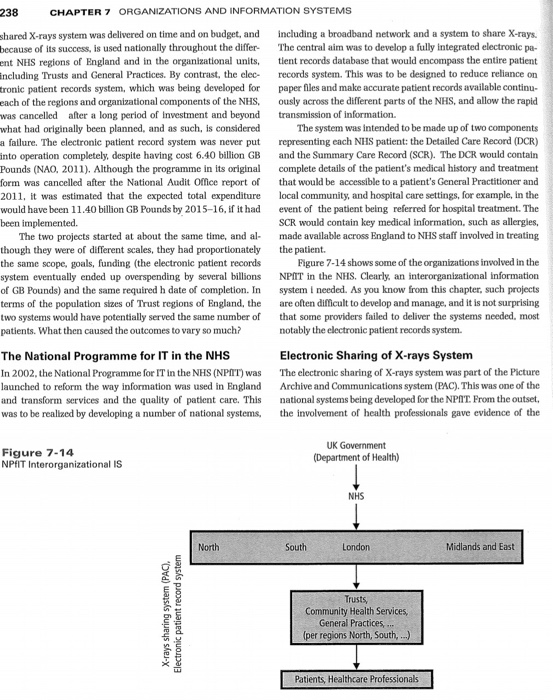
CASE STUDY 7 Interorganizational Is - The National Programme for IT in the NHS Experience The National Health Service (NHS) is the United Kingdom's publically funded healthcare system which serves the healthcare needs of its people, and proudly boasts its 'cradle-to-grave' and 'free-at-point-of-contact' credentials when compared to some other countries' similarly funded systems. It was founded in 1948, and continues to evolve organizationally, clinically, and in its development and use of information technologies, Just like its publicly and privately funded counterparts in Europe, Africa, Asia, the Middle East, Australia, and the US. Although overall control lies with the Department of Health, the NHS is divided into a number of regional centers, including London, North, and South, each of which has semi-autonomous control of health- care provision in an organizational structure, which includes Trusts, Community Health Services, and General Practices. The National Programme for IT in the NHS (NPAIT) was es- tablished to develop systems to electronically administer patient to information throughout the regions and their organizations. This required the development of interorganizational informa- tion systems. These parallel developments over an extended tion period of time provide us with an opportunity to learn from the experience of similar projects that had very different outcomes. Consider, for example, the development of the shared X-rays system and the electronic patient records system. The 238 CHAPTER 7 ORGANIZATIONS AND INFORMATION SYSTEMS shared X-rays system was delivered on time and on budget, and because of its success, is used nationally throughout the differ- ent NHS regions of England and in the organizational units, including Trusts and General Practices. By contrast, the elec- Fronic patient records system, which was being developed for each of the regions and organizational components of the NHS was cancelled after a long period of Investment and beyond what had originally been planned, and as such, is considered a failure. The electronic patient record system was never put into operation completely, despite having cost 6.40 billion GB Pounds (NAO, 2011). Although the programme in its original form was cancelled after the National Audit Office report of 2011, it was estimated that the expected total expenditure would have been 11.40 billion GB Pounds by 2015-16, if it had been implemented. The two projects started at about the same time, and al- though they were of different scales, they had proportionately the same scope, goals, funding (the electronic patient records system eventually ended up overspending by several billions of GB Pounds) and the same required h date of completion. In terms of the population sizes of Trust regions of England, the two systems would have potentially served the same number of patients. What then caused the outcomes to vary so much? including a broadband network and a system to share X-rays. The central aim was to develop a fully integrated electronic pa- tient records database that would encompass the entire patient records system. This was to be designed to reduce reliance on paper files and make accurate patient records available continu- ously across the different parts of the NHS, and allow the rapid transmission of information. The system was intended to be made up of two components representing each NHS patient: the Detailed Care Record (DCR) and the Summary Care Record (SCR). The DCR would contain complete details of the patient's medical history and treatment that would be accessible to a patient's General Practitioner and local community, and hospital care settings, for example, in the event of the patient being referred for hospital treatment. The SCR would contain key medical information, such as allergies, made available across England to NHS staff involved in treating the patient. Figure 7-14 shows some of the organizations involved in the NPIT in the NHS. Clearly, an interorganisational information system I needed. As you know from this chapter, such projects are often difficult to develop and manage, and it is not surprising that some providers failed to deliver the systems needed, most notably the electronic patient records system. The National Programme for IT in the NHS In 2002, the National Programme for IT in the NHS (NPAT) was launched to reform the way information was used in England and transform services and the quality of patient care. This was to be realized by developing a number of national systems, Electronic Sharing of X-rays System The electronic sharing of X-rays system was part of the Picture Archive and Communications system (PAC). This was one of the national systems being developed for the NPAT. From the outset, the involvement of health professionals gave evidence of the Figure 7-14 NPFIT Interorganizational IS UK Government (Department of Health) NHS North South London Midlands and East X-rays sharing system (PAC), Electronic patient record system Trusts Community Health Services, General Practices, ... (per regions North, South,...) Patients, Healthcare Professionals CHAPTER 7 ORG organization and planning of this project. This meant that the requirements for the system were clear and unambiguous, and thus grounded in clinical necessity versus political ambition. Importantly, an integral part of the programme involved the specification and implementation of a high-speed computer net- work linking all parts of the NHS organization, which enabled the relatively straightforward implementation of the X-rays sharing application. As was noted by Campion-Awwad in 2014, "The computer accessible X-ray system was delivered smoothly on budget and on time. The X-ray system was a rare product of consultation with health professionals, and was also assisted by plans that preceded the NPIIT. This system was added to the NPfIT well after the original specifications were approved, following a meet- ing between NPIIT and health professionals." By 2007, the system had been successfully rolled out and de- livered to all parts of the NHS organization with full buy-in with respect of all stakeholders, with their requirements in respect of the system being fully met clinically as well as organizationally. In these respects, the X-ray sharing system was an exemplar for other projects and systems within the NPAIT. Electronic Patient Record System The Electronic Patient Record System, on the other hand, was still far from completion by 2011 when the NAO reported on its progress in that year, some four years after the implementation of the X-rays sharing system. According to estimates given then, the work would have required a substantial further investment and would not have been complete until 2015-2016. Even after reducing the functional specification so as to bring forward the delivery of the system at reduced cost to the NHS organization, it became evident that timescales and cost savings would have been largely unaffected. By the time of the report, the Department of Health, and ultimately the government decided to dismantle and effectively cancel the programme in its NPIIT form. Since the cancellation of the project, a forensic examina- tion of the causes of the budget and time over-runs has taken place and the consensus is that at least four factors contributed to the abject failure of the programme: motives, buy-in, haste, and multi-sourcing. These could have been mitigated against had an interorganizational information system development - ERP, CRM, EAI - been undertaken from the start of the project Although praise-worthy in its ambition, the programme was motivated by government in a top-down fashion without fully consulting with IT experts, who would have been able to bring their project management skills and experience to bear. The lack of involvement of health professionals was found to be a major impediment as once systems and processes were being evaluated, there was a lack of buy-in from these end-users. Also, the speed with which contracts were awarded for the development of the system meant that planning, scope and de- liverables among other crucial project parameters fell seriously short. Having many contactors develop the system for different parts of the NHS organization meant that, in-theory, if any one contractor failed to deliver at any point in the programme, they could be substituted with another. However, in hindsight, this multi-sourcing approach proved to be near impossible to operate effectively, moving too far away from the tried-and-tested 'one customer, one service provider' model of delivery. Any one of these factors may have been recoverable if identified in reasonable time during the original project sched- ule. Unfortunately, this wasn't the case and when taken to- gether, the seeds of the programme's failure were sown at an early stage. QUESTIONS 7-11. Summarize the purpose and intended benefits of a healthcare exchange. 7-12. Explain why a healthcare exchange requires an interor- ganizational information system. system requires an interorganizational information system. 7-15. Using knowledge gained from this chapter, summarize the difficulties and challenges of developing interorga- nizational information systems, making references to how ERP, CRM and EAI systems may offer solutions to minimize these Step by Step Solution
There are 3 Steps involved in it
1 Expert Approved Answer
Step: 1 Unlock


Question Has Been Solved by an Expert!
Get step-by-step solutions from verified subject matter experts
Step: 2 Unlock
Step: 3 Unlock


