this is my resume and i need help updating based on job description
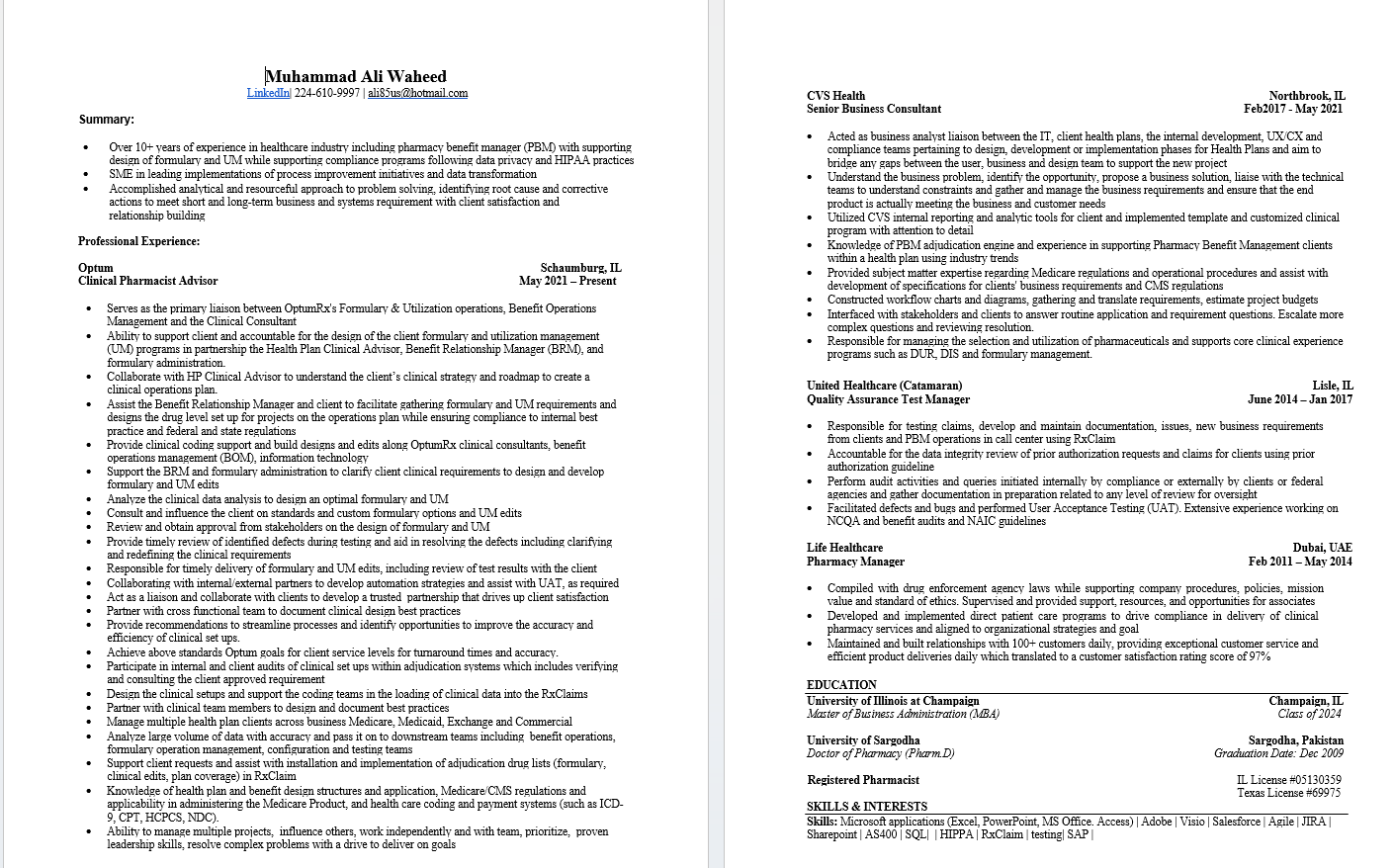
Muhammad Ali Waheed LinkedIn 224-610-9997 | ali8Sus@hotmail.com CVS Health Northbrook, IL Senior Business Consultant Feb2017 - May 202] Summary: . Acted as business analyst liaison between the IT, client health plans, the internal development, UX/CX and Over 10+ years of experience in healthcare industry including pharmacy benefit manager (PBM) with supporting compliance teams pertaining to design, development or implementation phases for Health Plans and aim to design of formulary and UM while supporting compliance programs following data privacy and HIPAA practices bridge any gaps between the user, business and design team to support the new project SME in leading implementations of process improvement mitiatives and data transformation Understand the business problem, identify the opportunity, propose a business solution, liaise with the technical Accomplished analytical and resourceful approach to problem solving, identifying root cause and corrective teams to understand constraints and gather and manage the business requirements and ensure that the end actions to meet short and long-term business and systems requirement with client satisfac product is actually meeting the business and customer needs relationship building Utilized CVS internal reporting and analytic tools for client and implemented template and customized clinical program with attention to detail Professional Experience: . Knowledge of PBM adjudication engine and experience in supporting Pharmacy Benefit Management clients within a health plan using industry trends Optum Schaumburg, IL . Clinical Pharmacist Advisor May 2021 - Present Provided subject matter expertise regarding Medicare regulations and operational procedures and assist with development of specifications for clients business requirements and CMS regulations Serves as the primary liaison between OptumRx's Formulary & Utilization operations, Benefit Operations Constructed workflow charts and diagrams, gathering and translate requirements, estimate project budgets . Management and the Clinical Consultant Interfaced with stakeholders and clients to answer routine application and requirement questions. Escalate more complex questions and reviewing resolution. Ability to support client and accountable for the design of the client formulary and utilization management Responsible for managing the selection and utilization of pharmaceuticals and supports core clinical experience (UM) programs in partnership the Health Plan Clinical Advisor, Benefit Relationship Manager (BRM), and programs such as DUR, DIS and formulary management. formulary administration. Collaborate with HP Clinical Advisor to understand the client's clinical strategy and roadmap to create a clinical operations plan. United Healthcare (Catamaran) Lisle, IL Assist the Benefit Relationship Manager and client to facilitate gathering formulary and UM requirements and Quality Assurance Test Manager June 2014 - Jan 2017 designs the drug level set up for projects on the operations plan while ensuring compliance to internal best practice and federal and state regulations . Responsible for testing claims, develop and maintain documentation, issues, new business requirements Provide clinical coding support and build designs and edits along OptumRx clinical consultants, benefit from clients and PBM operations in call center using RxClaim operations management (BOM), information technology Accountable for the data integrity review of prior authorization requests and claims for clients using prior Support the BRM and formulary administration to clarify client clinical requirements to design and develop authorization guideline formulary and UM edits Perform audit activities and queries initiated internally by compliance or externally by clients or federal Analyze the clinical data analysis to design an optimal formulary and UM agencies and gather documentation in preparation related to any level of review for oversight Consult and influence the client on standards and custom formulary options and UM edits Facilitated defects and bugs and performed User Acceptance Testing (UAT). Extensive experience working on Review and obtain approval from stakeholders on the design of formulary and UM NCQA and benefit audits and NAIC guidelines Provide timely review of identified defects during testing and aid in resolving the defects including clarifying Life Healthcare Dubai, UAE and redefining the clinical requirements Feb 2011 - May 2014 Responsible for timely delivery of formulary and UM edits, including review of test results with the client Pharmacy Manager Collaborating with internal/external partners to develop automation strategies and assist with UAT, as required . Compiled with drug enforcement agency laws while supporting company procedures, policies, mission Act as a liaison and collaborate with clients to develop a trusted partnership that drives up client satisfaction value and standard of ethics. Supervised and provided support, resources, and opportunities for associates Partner with cross functional team to document clinical design best practices . Developed and implemented direct patient care programs to drive compliance in delivery of clinical Provide recommendations to streamline processes and identify opportunities to improve the accuracy and pharmacy services and aligned to organizational strategies and goal efficiency of clinical set ups. Maintained and built relationships with 100+ customers daily, providing exceptional customer service and Achieve above standards Optum goals for client service levels for turnaround times and accuracy. efficient product deliveries daily which translated to a customer satisfaction rating score of 97% Participate in internal and client audits of clinical set ups within adjudication systems which includes verifying and consulting the client approved requirement EDUCATION Design the clinical setups and support the coding teams in the loading of clinical data into the RxClaims University of Illinois at Champaign Champaign, IL Partner with clinical team members to design and document best practices Master of Business Administration (MBA) Class of 2024 Manage multiple health plan clients across business Medicare, Medicaid, Exchange and Commercial Analyze large volume of data with accuracy and pass it on to downstream teams including benefit operations, University of Sargodha Sargodha, Pakistan formulary operation management, configuration and testing teams Doctor of Pharmacy (Pharm. D) Graduation Date: Dec 2009 Support client requests and assist with installation and implementation of adjudication drug lists (formulary, clinical edits, plan coverage) in RxClaim Registered Pharmacist IL License #05130359 Knowledge of health plan and benefit design structures and application, Medicare CMS regulations and Texas License #69975 applicability in administering the Medicare Product, and health care coding and payment systems (such as ICD- SKILLS & INTERESTS 9, CPT, HCPCS, NDC). Skills: Microsoft applications (Excel, PowerPoint, MS Office. Access) | Adobe | Visio | Salesforce | Agile | Ability to manage multiple projects, influence others, work independently and with team, prioritize, proven Sharepoint | AS400 | SQL| | HIPPA | RxClaim | testing| SAP | leadership skills, resolve complex problems with a drive to deliver on goals