Jill, the CEO of Redmond Medical Center, and her assistant, Joe, attended the American College of Healthcare
Question:
Jill, the CEO of Redmond Medical Center, and her assistant, Joe, attended the American College of Healthcare Executives’ (ACHE) annual Congress last week and, upon comparing notes, they concurred that moving healthcare to “value-based care” appeared to be the direction of most of the country’s providers. As defined at the ACHE meeting, value-based care models focus on the value received by patients by rewarding better outcomes, which moves a health provider away from the traditional fee-for-service model that rewards for more volume.
Few systems have moved away from the volume, fee-for-service model to a value-based system. In 2016, only 27 percent of healthcare provider organizations had experimented with or completed value-based pilot programs (Sanicola 2017). However, employers, health insurance companies, and government purchasers have begun to encourage providers to transition to value-based payment models. For example, the Centers for Medicare & Medicaid Services (CMS) had implemented value-based programs primarily for Medicare patients with the goal to link provider performance of quality measures to provider payment. These included the following:
• Hospital Value-Based Purchasing Program
• Hospital Readmission Reduction Program
• Value Modifier Program (also called the Physician Value-Based Modifier, or PVBM)
• Hospital-Acquired Condition Reduction Program
• End-Stage Renal Disease Quality Initiative Program
• Skilled Nursing Facility Value-Based Program
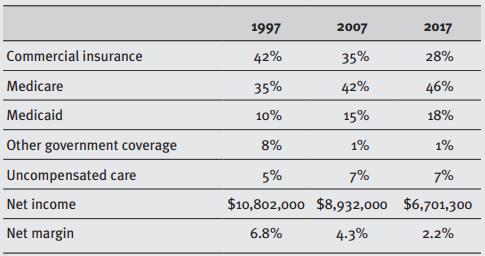
• Home Health Value-Based Program Until now, the hospital had not put much effort in addressing the requirements of value-based programs, but, as can be seen below, the medical center has seen a great shift in its patient population and profitability. In the past 20 years, the commercial insurance patient market has shrunk by one-third (down 14 percent), while governmental paid patients have gone from 53 percent to 65 percent of all patients. Concurrently, net income decreased by over $4 million and the net margin from 6.8 percent to 2.2 percent.
Questions
1. What could Jill and Joe do to understand their level of preparedness for change more fully?
2. Who would be the key stakeholders for the proposed changes?
3. Why should Jill and Joe expect resistance to this type of change and what could they do to address it?
4. What should they do before they decide to go ahead with this change?
Step by Step Answer:

Strategic Healthcare Management Planning And Execution
ISBN: 9781640553651
3rd Edition
Authors: Stephen L. Walston PhD