Question: 2. You are asked to develop a policy to reduce the risk of communication failure. 2.1 Explain the difference between a policy and a procedure.
2. You are asked to develop a policy to reduce the risk of communication failure.
2.1 Explain the difference between a policy and a procedure. (2)
2.2 Explain how a bureaucratic design might impede communication between different departments e.g. medical and nursing departments. In your answer, refer to at least two limitations of the bureaucratic design. (4)
2.3 Discuss two benefits that demonstrates why the bureaucratic design remains prevalent in large organizations. (2)
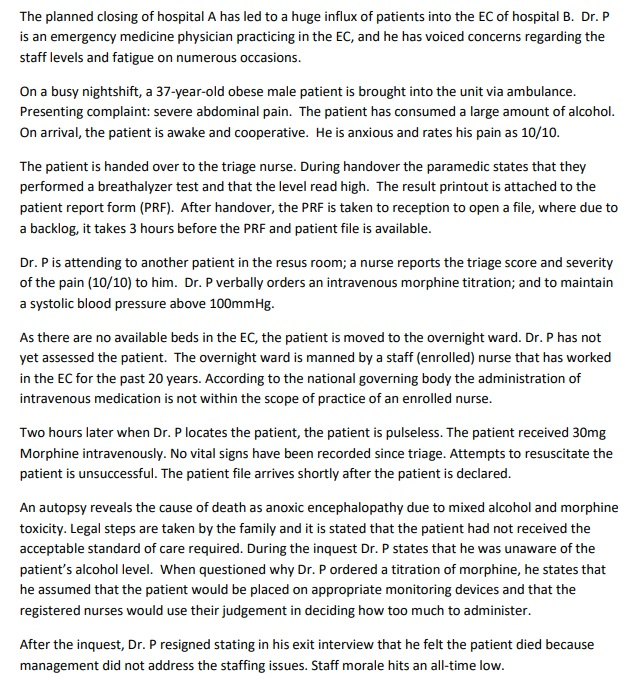
The planned closing of hospital A has led to a huge influx of patients into the EC of hospital B. Dr. P is an emergency medicine physician practicing in the EC, and he has voiced concerns regarding the staff levels and fatigue on numerous occasions. On a busy nightshift, a 37-year-old obese male patient is brought into the unit via ambulance. Presenting complaint: severe abdominal pain. The patient has consumed a large amount of alcohol. On arrival, the patient is awake and cooperative. He is anxious and rates his pain as 10/10. The patient is handed over to the triage nurse. During handover the paramedic states that they performed a breathalyzer test and that the level read high. The result printout is attached to the patient report form (PRF). After handover, the PRF is taken to reception to open a file, where due to a backlog, it takes 3 hours before the PRF and patient file is available. Dr. Pis attending to another patient in the resus room; a nurse reports the triage score and severity of the pain (10/10) to him. Dr. P verbally orders an intravenous morphine titration; and to maintain a systolic blood pressure above 100mmHg. As there are no available beds in the EC, the patient is moved to the overnight ward. Dr. P has not yet assessed the patient. The overnight ward is manned by a staff (enrolled) nurse that has worked in the EC for the past 20 years. According to the national governing body the administration of intravenous medication is not within the scope of practice of an enrolled nurse. Two hours later when Dr. P locates the patient, the patient is pulseless. The patient received 30mg Morphine intravenously. No vital signs have been recorded since triage. Attempts to resuscitate the patient is unsuccessful. The patient file arrives shortly after the patient is declared. An autopsy reveals the cause of death as anoxic encephalopathy due to mixed alcohol and morphine toxicity. Legal steps are taken by the family and it is stated that the patient had not received the acceptable standard of care required. During the inquest Dr. P states that he was unaware of the patient's alcohol level. When questioned why Dr. P ordered a titration of morphine, he states that he assumed that the patient would be placed on appropriate monitoring devices and that the registered nurses would use their judgement in deciding how too much to administer. After the inquest, Dr. P resigned stating in his exit interview that he felt the patient died because management did not address the staffing issues. Staff morale hits an all-time lowStep by Step Solution
There are 3 Steps involved in it

Get step-by-step solutions from verified subject matter experts


