Question: Based on information available, assess the general strategic planning approach/process used by each of the healthcare organizations: Case 5: Webster Health System ebster Health System
- Based on information available, assess the general strategic planning approach/process used by each of the healthcare organizations:
- Case 5: Webster Health System
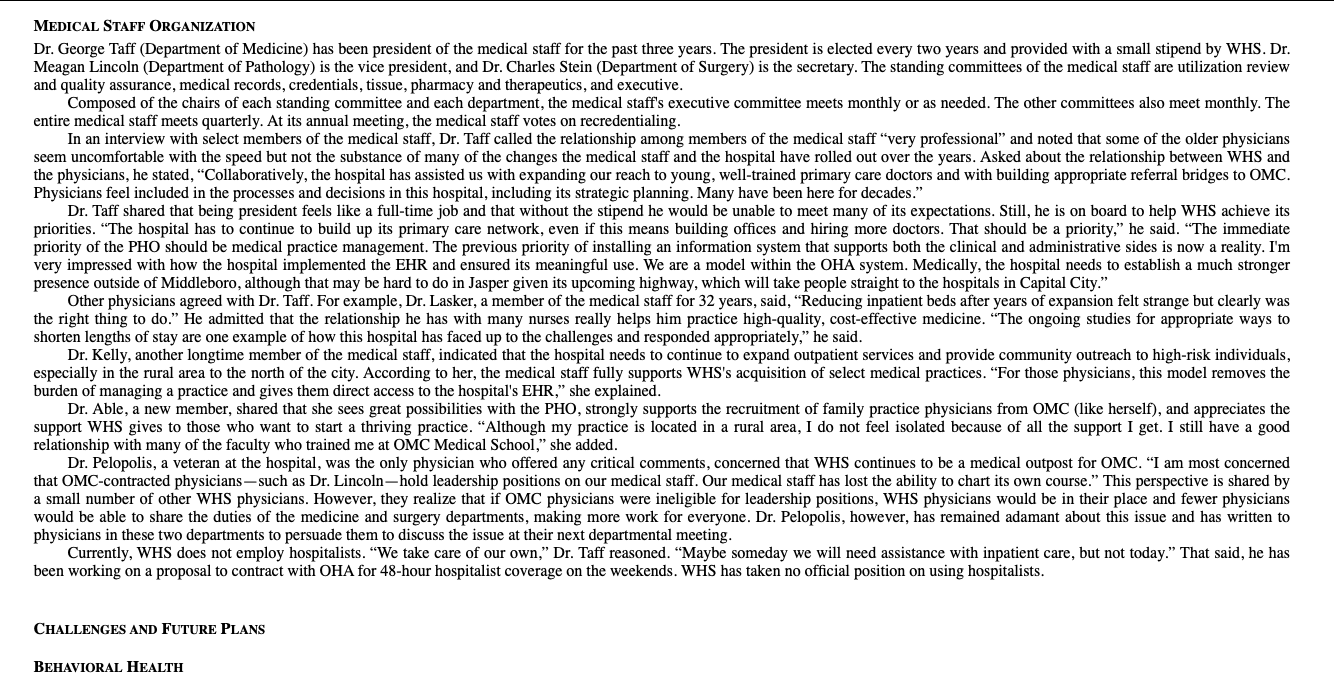
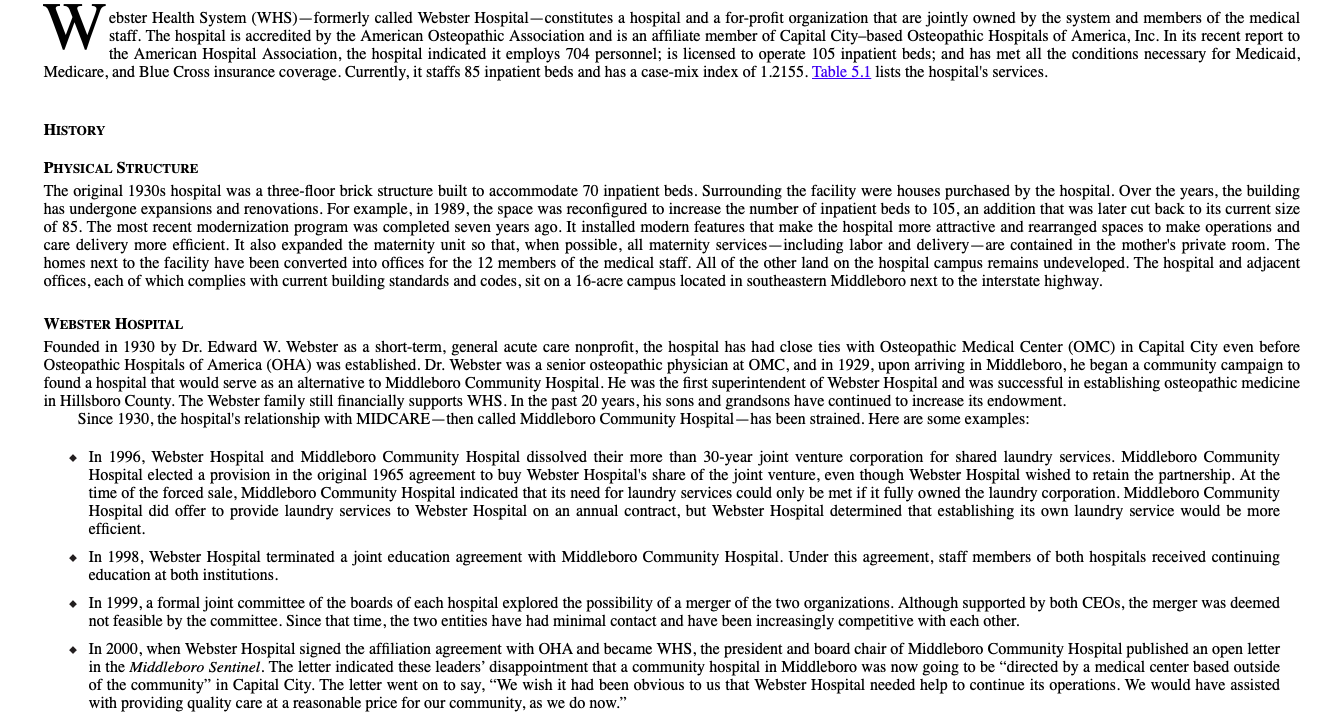
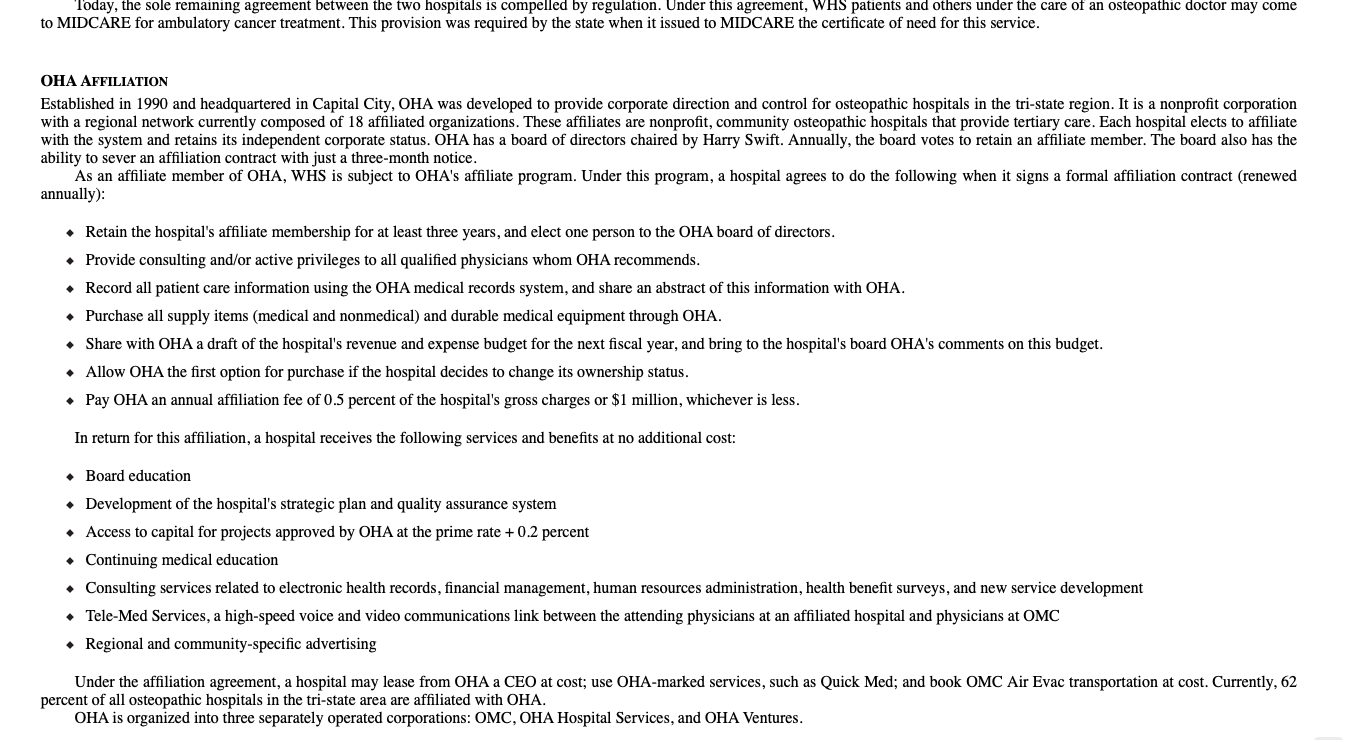
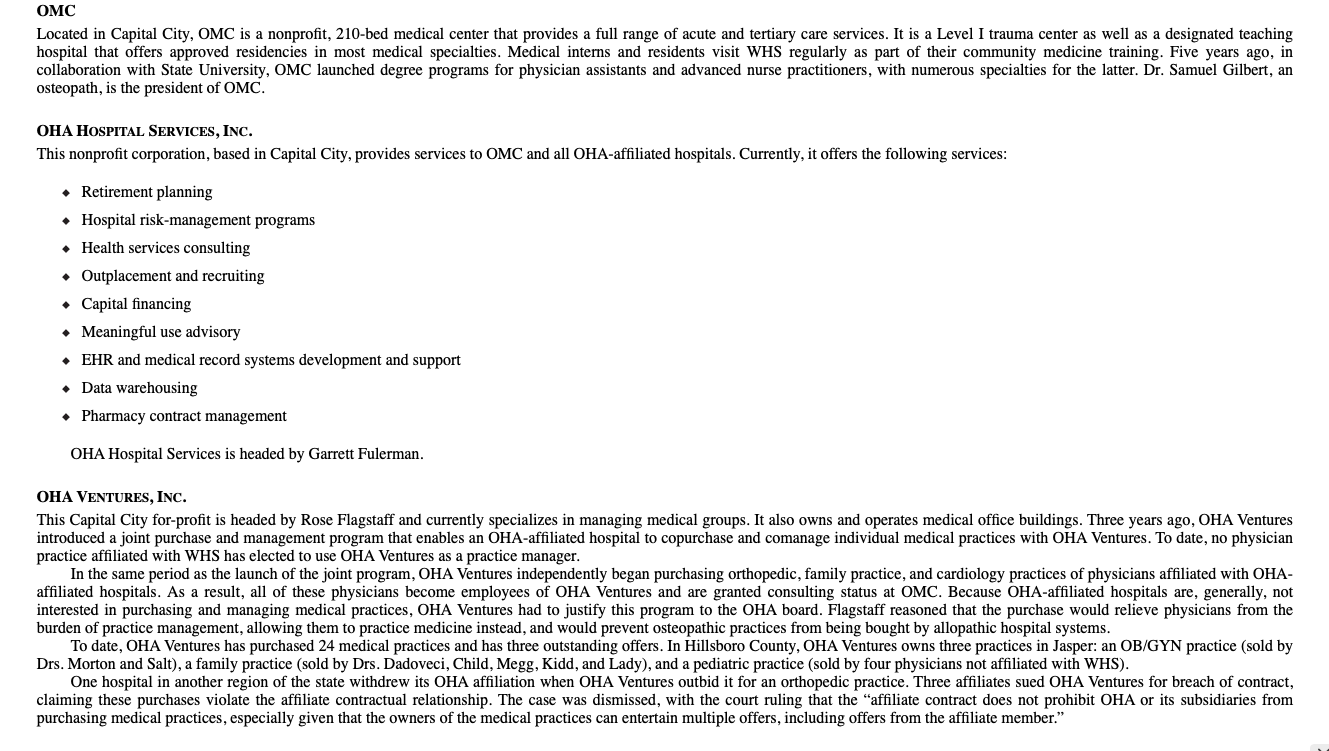
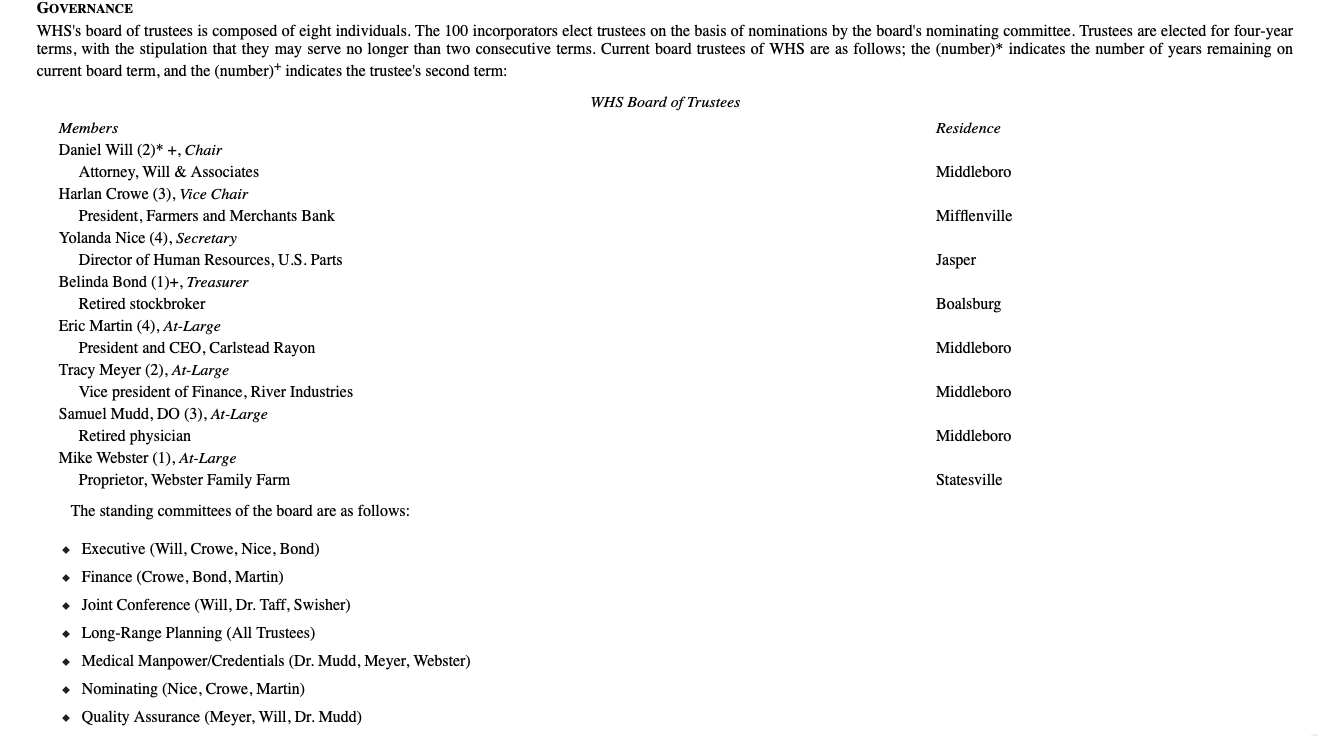
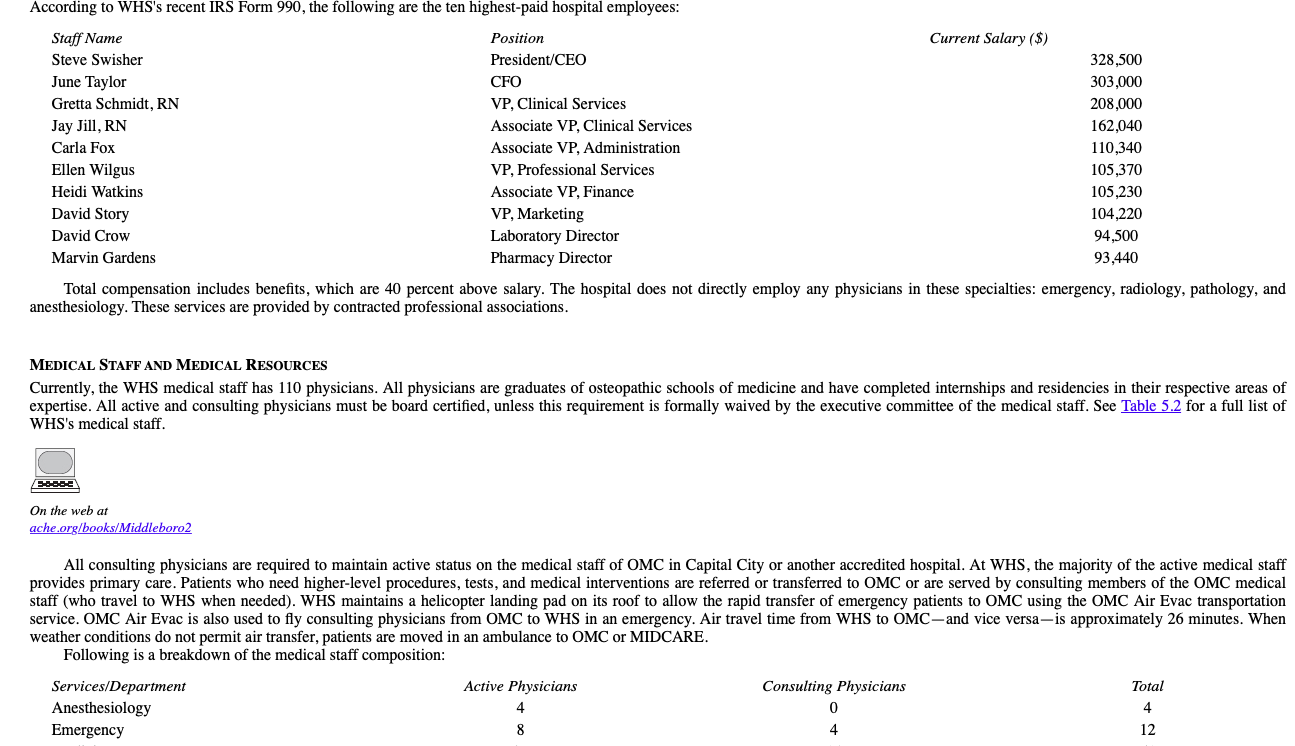
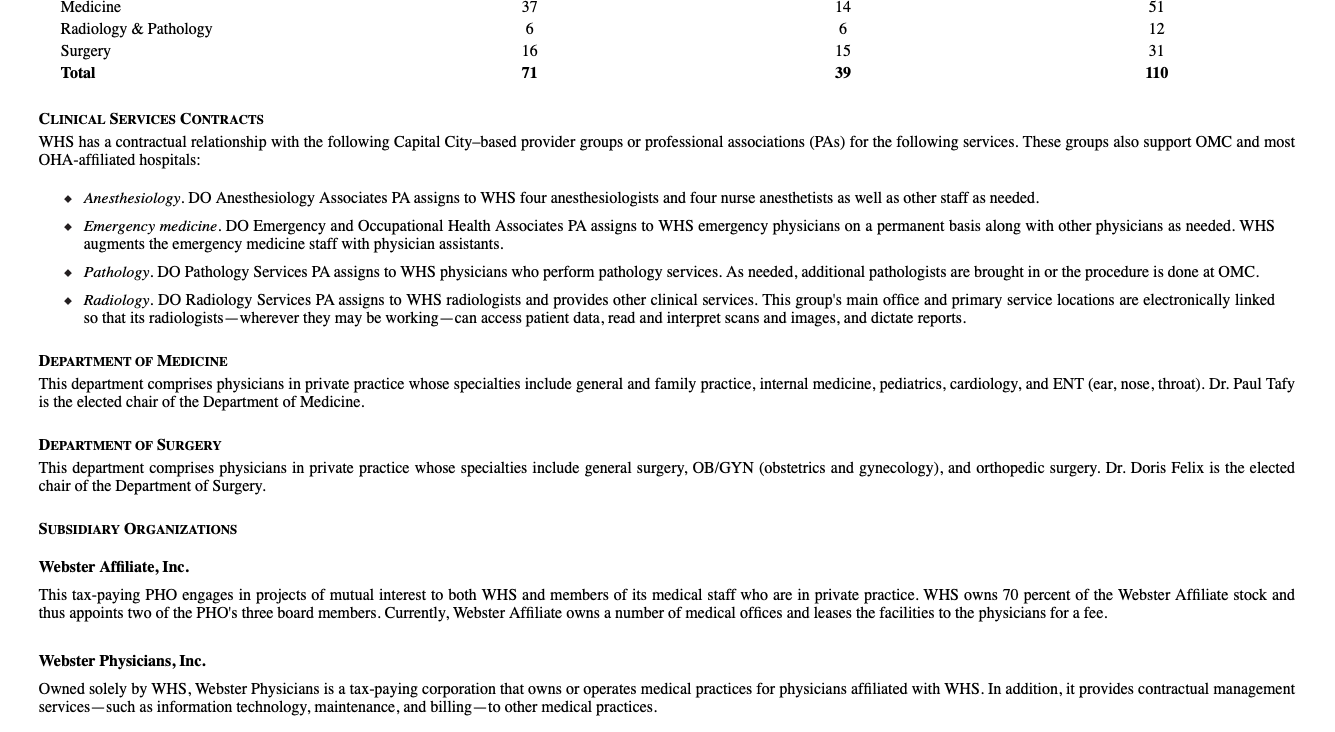
ebster Health System (WHS), formerly called Webster Hospital - constitutes a hospital and a for-profit organization that are jointly owned by the system and members of the medical staff. The hospital is accredited by the American Osteopathic Association and is an affiliate member of Capital City-based Osteopathic Hospitals of America, Inc. In its recent report to the American Hospital Association, the hospital indicated it employs 704 personnel; is licensed to operate 105 inpatient beds; and has met all the conditions necessary for Medicaid, Medicare, and Blue Cross insurance coverage. Currently, it staffs 85 inpatient beds and has a case-mix index of 1.2155. Table 5.1 lists the hospital's services. W HISTORY PHYSICAL STRUCTURE The original 1930s hospital was a three-floor brick structure built to accommodate 70 inpatient beds. Surrounding the facility were houses purchased by the hospital. Over the years, the building has undergone expansions and renovations. For example, in 1989, the space was reconfigured to increase the number of inpatient beds to 105, an addition that was later cut back to its current size of 85. The most recent modernization program was completed seven years ago. It installed modern features that make the hospital more attractive and rearranged spaces to make operations and care delivery more efficient. It also expanded the maternity unit so that, when possible, all maternity services, including labor and delivery-are contained in the mother's private room. The homes next to the facility have been converted into offices for the 12 members of the medical staff. All of the other land on the hospital campus remains undeveloped. The hospital and adjacent offices, each of which complies with current building standards and codes, sit on a 16-acre campus located in southeastern Middleboro next to the interstate highway. WEBSTER HOSPITAL Founded in 1930 by Dr. Edward W. Webster as a short-term, general acute care nonprofit, the hospital has had close ties with Osteopathic Medical Center (OMC) in Capital City even before Osteopathic Hospitals of America (OHA) was established. Dr. Webster was a senior osteopathic physician at OMC, and in 1929, upon arriving in Middleboro, he began a community campaign to found a hospital that would serve as an alternative to Middleboro Community Hospital. He was the first superintendent of Webster Hospital and was successful in establishing osteopathic medicine in Hillsboro County. The Webster family still financially supports WHS. In the past 20 years, his sons and grandsons have continued to increase its endowment. Since 1930, the hospital's relationship with MIDCARE,then called Middleboro Community Hospital - has been strained. Here are some examples: In 1996, Webster Hospital and Middleboro Community Hospital dissolved their more than 30-year joint venture corporation for shared laundry services. Middleboro Community Hospital elected a provision in the original 1965 agreement to buy Webster Hospital's share of the joint venture, even though Webster Hospital wished to retain the partnership. At the time of the forced sale, Middleboro Community Hospital indicated that its need for laundry services could only be met if it fully owned the laundry corporation. Middleboro Community Hospital did offer to provide laundry services to Webster Hospital on an annual contract, but Webster Hospital determined that establishing its own laundry service would be more efficient. . In 1998, Webster Hospital terminated a joint education agreement with Middleboro Community Hospital. Under this agreement, staff members of both hospitals received continuing education at both institutions. In 1999, a formal joint committee of the boards of each hospital explored the possibility of a merger of the two organizations. Although supported by both CEOs, the merger was deemed not feasible by the committee. Since that time, the two entities have had minimal contact and have been increasingly competitive with each other. . In 2000, when Webster Hospital signed the affiliation agreement with OHA and became WHS, the president and board chair of Middleboro Community Hospital published an open letter in the Middleboro Sentinel. The letter indicated these leaders' disappointment that a community hospital in Middleboro was now going to be directed by a medical center based outside of the community" in Capital City. The letter went on to say, "We wish it had been obvious to us that Webster Hospital needed help to continue its operations. We would have assisted with providing quality care at a reasonable price for our community, as we do now." Today, the sole remaining agreement between the two hospitals is compelled by regulation. Under this agreement, WHS patients and others under the care of an osteopathic doctor may come to MIDCARE for ambulatory cancer treatment. This provision was required by the state when it issued to MIDCARE the certificate of need for this service. OHA AFFILIATION Established in 1990 and headquartered in Capital City, OHA was developed to provide corporate direction and control for osteopathic hospitals in the tri-state region. It is a nonprofit corporation with a regional network currently composed of 18 affiliated organizations. These affiliates are nonprofit, community osteopathic hospitals that provide tertiary care. Each hospital elects to affiliate with the system and retains its independent corporate status. OHA has a board of directors chaired by Harry Swift. Annually, the board votes to retain an affiliate member. The board also has the ability to sever an affiliation contract with just a three-month notice. As an affiliate member of OHA, WHS is subject to OHA's affiliate program. Under this program, a hospital agrees to do the following when it signs a formal affiliation contract (renewed annually): Retain the hospital's affiliate membership for at least three years, and elect one person to the OHA board of directors. Provide consulting and/or active privileges to all qualified physicians whom OHA recommends. Record all patient care information using the OHA medical records system, and share an abstract of this information with OHA. Purchase all supply items (medical and nonmedical) and durable medical equipment through OHA. Share with OHA a draft of the hospital's revenue and expense budget for the next fiscal year, and bring to the hospital's board OHA's comments on this budget. Allow OHA the first option for purchase if the hospital decides to change its ownership status. Pay OHA an annual affiliation fee of 0.5 percent of the hospital's gross charges or $1 million, whichever is less. In return for this affiliation, a hospital receives the following services and benefits at no additional cost: Board education Development of the hospital's strategic plan and quality assurance system Access to capital for projects approved by OHA at the prime rate +0.2 percent Continuing medical education . Consulting services related to electronic health records, financial management, human resources administration, health benefit surveys, and new service development Tele-Med Services, a high-speed voice and video communications link between the attending physicians at an affiliated hospital and physicians at OMC Regional and community-specific advertising Under the affiliation agreement, a hospital may lease from OHA a CEO at cost; use OHA-marked services, such as Quick Med; and book OMC Air Evac transportation at cost. Currently, 62 percent of all osteopathic hospitals the tri-state area are affiliated with OHA. OHA is organized into three separately operated corporations: OMC, OHA Hospital Services, and OHA Ventures. OMC Located in Capital City, OMC is a nonprofit, 210-bed medical center that provides a full range of acute and tertiary care services. It is a Level I trauma center as well as a designated teaching hospital that offers approved residencies in most medical specialties. Medical interns and residents visit WHS regularly as part of their community medicine training. Five years ago, in collaboration with State University, OMC launched degree programs for physician assistants and advanced nurse practitioners, with numerous specialties for the latter. Dr. Samuel Gilbert, an osteopath, is the president of OMC. OHA HOSPITAL SERVICES, INC. This nonprofit corporation, based in Capital City, provides services to OMC and all OHA-affiliated hospitals. Currently, it offers the following services: . Retirement planning Hospital risk-management programs Health services consulting Outplacement and recruiting Capital financing Meaningful use advisory EHR and medical record systems development and support Data warehousing Pharmacy contract management OHA Hospital Services is headed by Garrett Fulerman. OHA VENTURES, INC. This Capital City for-profit is headed by Rose Flagstaff and currently specializes in managing medical groups. It also owns and operates medical office buildings. Three years ago, OHA Ventures introduced a joint purchase and management program that enables an OHA-affiliated hospital to copurchase and comanage individual medical practices with OHA Ventures. To date, no physician practice affiliated with WHS has elected to use OHA Ventures as a practice manager. In the same period as the launch of the joint program, OHA Ventures independently began purchasing orthopedic, family practice, and cardiology practices of physicians affiliated with OHA- affiliated hospitals. As a result, all of these physicians become employees of OHA Ventures and are granted consulting status at OMC. Because OHA-affiliated hospitals are, generally, not interested in purchasing and managing medical practices, OHA Ventures had to justify this program to the OHA board. Flagstaff reasoned that the purchase would relieve physicians from the burden of practice management, allowing them to practice medicine instead, and would prevent osteopathic practices from being bought by allopathic hospital systems. To date, OHA Ventures has purchased 24 medical practices and has three outstanding offers. In Hillsboro County, OHA Ventures owns three practices in Jasper: an OB/GYN practice (sold by Drs. Morton and Salt), a family practice (sold by Drs. Dadoveci, Child, Megg, Kidd, and Lady), and a pediatric practice (sold by four physicians not affiliated with WHS). One hospital in another region of the state withdrew its OHA affiliation when OHA Ventures outbid it for an orthopedic practice. Three affiliates sued OHA Ventures for breach of contract, claiming these purchases violate the affiliate contractual relationship. The case was dismissed, with the court ruling that the "affiliate contract does not prohibit OHA or its subsidiaries from purchasing medical practices, especially given that the owners of the medical practices can entertain multiple offers, including offers from the affiliate member." GOVERNANCE WHS's board of trustees is composed of eight individuals. The 100 incorporators elect trustees on the basis of nominations by the board's nominating committee. Trustees are elected for four-year terms, with the stipulation that they may serve no longer than two consecutive terms. Current board trustees of WHS are as follows; the (number)* indicates the number of years remaining on current board term, and the number)+ indicates the trustee's second term: WHS Board of Trustees Residence Middleboro Mifflenville Jasper Boalsburg Members Daniel Will (2)* +, Chair Attorney, Will & Associates Harlan Crowe (3), Vice Chair President, Farmers and Merchants Bank Yolanda Nice (4), Secretary Director of Human Resources, U.S. Parts Belinda Bond (1)+, Treasurer Retired stockbroker Eric Martin (4), At-Large President and CEO, Carlstead Rayon Tracy Meyer (2), At-Large Vice president of Finance, River Industries Samuel Mudd, DO (3), At-Large Retired physician Mike Webster (1), At-Large Proprietor, Webster Family Farm The standing committees of the board are as follows: Middleboro Middleboro Middleboro Statesville Executive (Will, Crowe, Nice, Bond) Finance (Crowe, Bond, Martin) Joint Conference (Will, Dr. Taff, Swisher) Long-Range Planning (All Trustees) Medical Manpower/Credentials (Dr. Mudd, Meyer, Webster) Nominating (Nice, Crowe, Martin) Quality Assurance (Meyer, Will, Dr. Mudd) The board meets monthly, the executive committee meets twice a month, and other committees meet as needed (usually monthly). Every December, the board-along with the hospital auxiliary - sponsors a hospital fund-raising event called Holiday Ball at the Middleboro Golf Club. MANAGEMENT TEAM AND ORGANIZATIONAL STRUCTURE PRESIDENT AND CEO Steve Swisher, CPA, was promoted to president and CEO nine months ago. Prior to this appointment, he was vice president of Administrative Services and chief financial officer (CFO) at WHS for 14 years. He holds a bachelor in accounting and a master of business administration from a midwestern university and is a member of the Healthcare Financial Management Association. Before coming to WHS, he was a senior fiscal analyst at Blue Cross and Blue Shield in Capital City. The position of president and CEO became vacant when the well-loved and respected Edith Masterman retired from the job four years ago. WHS used a national executive search firm to identify qualified candidates. The first search yielded no candidates acceptable to the board, but the second search resulted in the hiring of Stella MacArthur. Twelve months later, however, she reached a mutual agreement with the board and resigned from the post. The board offered no reason for her immediate departure. During another lengthy search, Swisher was appointed acting president. When interviewed, Swisher noted the board's concerns regarding changing market dynamics, especially in Jasper; the need to recruit new physicians for WHS's primary markets; the potential addition of specialized services; the system's financial challenges; and the development of a regional accountable care organization. He offered a "that's confidential in response to reports that WHS's affiliation with OHA has become difficult, but he said this to clear up other rumors: "Our strength is our people, who are highly skilled and dedicated to our mission. We focus on keeping them happy, so I'm not aware of any behind-the-scenes union activity among our clerical and administrative staff. In regards to the turmoil associated with my office, there's none-no turmoil. We stumbled a few times during the recruitment process, but I think that may be due to our inexperience. Edith was so good at this job for so long that we relied too much on her instead of developing our own competencies and ensuring our policies match our changing needs. For example, we don't have an experienced governing board. That's because our bylaws dictate we remove the experienced trustees after serving only two terms on the board, so we lose the organizational knowledge and insights they gained during their tenure. That holds us back, and we have to address that and other issues if we want to create a strong vision and strategies for the future." VICE PRESIDENT OF ADMINISTRATIVE SERVICES AND CFO June Taylor, CPA, replaced Swisher in this position. She was promoted from the position of deputy chief fiscal officer, where she had been for ten years. She holds a bachelor in accounting and a master of business administration from State University and is a member of the Healthcare Financial Management Association. As Swisher's direct report, she has extensive responsibilities, including overseeing these departments: Admitting, Business Office, Central Supply, Housekeeping, Laundry, Maintenance, Medical Records, Personnel, Purchasing, Security, and Telecommunications. In addition, Taylor is in charge of a laundry service contract between WHS and Hillsboro County Health Department. Several years ago, when WHS began searching for clients to use its excess laundry capacity (caused by the decrease in inpatient days), Taylor developed a contractual program that has WHS providing laundry services to Manorhaven, the long-term care facility owned and operated by Hillsboro County Health Department. She indicated that this contract, aside from being good business, keeps the hospital's laundry service an efficient operation with its current level of staffing. Another one of her many duties is as chief personnel officer, which has become an almost full-time job." She said, Our HR staff have had a hard time filling openings because there seems to be a lack of qualified, acceptable professionals in our area. We're working hard to attract them." Although Taylor remains optimistic about the future, she has worries. The hospital's inpatient capacity has gotten about as small as it should," she said. "Too much smaller, and it will become less efficient." As a result, she advocates a competitive strategy to capture ambulatory and inpatient market share historically served by MIDCARE. The good news is the hospital has a win-win relationship with the staff, including the medical staff. They know our needs, we know theirs, and we are committed to joint success," she added. Five years ago, WHS installed an electronic health record system, with full support from OHA. All medical practices owned by WHS-through Webster Physicians are connected to the system, while other affiliated practices can access the system by purchasing or leasing the software from WHS or OHA and then logging in through an online portal. Technical oversight of the system is provided by a private contractor and OHA Hospital Services. Taylor does not think the hospital needs a chief information systems officer at this time: Our current arrangement with OHA for consulting services seems to be working well. We have their expertise, and the contractor is very responsive to our needs." VICE PRESIDENT OF PROFESSIONAL SERVICES Ellen Wilgus has been employed by WHS for 15 years and was director of Physical Therapy right before her appointment as vice president. She holds a bachelor in physical therapy from State University. She has served as president of the state chapter of the American Physical Therapy Association and remains active in professional organizations related to physical therapy and rehabilitation Wilgus reports to the president and has responsibility for the following departments: Anesthesiology, Dietary, Laboratory, Pharmacy, Physical Therapy, Radiology, Respiratory Therapy, and Social Services. The ever-increasing complexity of hospital management and the greater competition from MIDCARE are among her top concerns; she thinks WHS faces an uncertain future, even with its affiliation with OHA. The hospital's decision to retain extra staff, and retrain them when needed, as it changes its primary orientation away from inpatient services made all the difference in the world, she explained. Staff became creative problem solvers because they knew they were not going to lose their jobs. She also indicated feeling supported by her hardworking department heads and especially proud that the most recent accreditation review found no significant deficiencies in any of the departments she oversees. Years ago, Wilgus headed the management task force that implemented the maternity unit redesign and expansion. For her exemplary performance on the task force, she earned an official commendation from the medical staff as well as a special recognition from the board and the former president. Currently, she leads the continuous quality improvement team's effort to shorten the length of inpatient hospital stays per diagnosis-related group. VICE PRESIDENT OF CLINICAL SERVICES Gretta Schmidt, RN, was hired to replace a retiring vice president. Prior to coming to WHS, she held numerous nursing positions at MIDCARE, including associate director of nursing, making her the first senior management member to have worked for a direct competitor; her selection was a unanimous decision approved by leadership. She graduated from MIDCARE School of Nursing, has a bachelor and master in nursing from State University, and is active in the state nursing association. Like the other vice presidents, Schmidt reports to the president and is in charge of multiple departments, including Clinical Education, Pediatrics, Intensive Care, Medical Surgical Unit I, Medical Surgical Unit II, Medical Surgical Unit III, Emergency and Outpatient Departments, and Staff Development. WHS maintains a high nurse-patient ratio and is making progress in achieving an all-RN (registered nurse) nursing staff, something she is concentrating on. When interviewed, Schmidt was careful with her remarks about MIDCARE, stating, I'm unsure about the real issues between MIDCARE and this hospital. I sure am very impressed, though, by the high clinical competence of the nursing staff here. Nurse turnover is not as big an issue here as it is at MIDCARE. She is equally complimentary of the professional relationship between physicians and nurses. Although there is no formal joint practice program, most aspects of joint practice characterize the nurse-physician relationship, she said. VICE PRESIDENT OF MARKETING David Story, who is from a prominent family in Middleboro, has been the marketing head at WHS for 12 years and, before that was deputy director of marketing for a durable medical equipment firm in Capital City. He holds a liberal arts degree and a master of health administration from an eastern university and is a member of the American College of Healthcare Executives (ACHE). His tenure at WHS has been productive from the beginning, and these successes have not been limited to marketing. He secured the certificate of need for the hospital's first CT (computed tomography) scanner. He recruited a number of physicians, many of whom are still on the medical staff. He, along with Swisher, negotiated a long-term financial loan with OMC to finance a project. Currently, he is working with Schmidt and the medical staff to examine the feasibility of establishing a women's health center at WHS. He also serves as the director of Webster Affiliate, Inc., the physician-hospital organization (PHO) he created to facilitate joint ventures - including joint medical practices-between the hospital and members of the medical staff. MANAGEMENT INTERN This advisory staff position is currently held by Justin Perkins, who recently earned a master of business and hospital administration from an eastern university and is completing a 24-month postgraduate fellowship program recognized by ACHE. Under the terms of this fellowship, the hospital has made no long-term employment commitment to him. A son of an osteopathic physician, Perkins was a unit manager at a large medical center before entering graduate school. Currently, he provides staff support to the president as well as to several board and hospital committees and has been managing WHS's Employee of the Month/Year program. He is a member of ACHE. INTERNAL REVENUE SERVICE FORM 990 DISCLOSURE According to WHS's recent IRS Form 990, the following are the ten highest-paid hospital employees: Staff Name Position Current Salary($) Steve Swisher President/CEO 328,500 June Taylor CFO 303,000 Gretta Schmidt, RN VP, Clinical Services 208,000 Jay Jill, RN Associate VP, Clinical Services 162,040 Carla Fox Associate VP, Administration 110,340 Ellen Wilgus VP, Professional Services 105,370 Heidi Watkins Associate VP, Finance 105,230 David Story VP, Marketing 104,220 David Crow Laboratory Director 94,500 Marvin Gardens Pharmacy Director 93,440 Total compensation includes benefits, which are 40 percent above salary. The hospital does not directly employ any physicians in these specialties: emergency, radiology, pathology, and anesthesiology. These services are provided by contracted professional associations. MEDICAL STAFF AND MEDICAL RESOURCES Currently, the WHS medical staff has 110 physicians. All physicians are graduates of osteopathic schools of medicine and have completed internships and residencies in their respective areas of expertise. All active and consulting physicians must be board certified, unless this requirement is formally waived by the executive committee of the medical staff. See Table 5.2 for a full list of WHS's medical staff. On the web at ache.org/books/Middleboro2 All consulting physicians are required to maintain active status on the medical staff of OMC in Capital City or another accredited hospital. At WHS, the majority of the active medical staff provides primary care. Patients who need higher-level procedures, tests, and medical interventions are referred or transferred to OMC or are served by consulting members of the OMC medical staff (who travel to WHS when needed). WHS maintains a helicopter landing pad on its roof to allow the rapid transfer of emergency patients to OMC using the OMC Air Evac transportation service. OMC Air Evac is also used to fly consulting physicians from OMC to WHS in an emergency. Air travel time from WHS to OMCand vice versais approximately 26 minutes. When weather conditions do not permit air transfer, patients are moved in an ambulance to OMC or MIDCARE. Following is a breakdown of the medical staff composition: Services/Department Active Physicians Consulting Physicians Total Anesthesiology Emergency 12 4 0 4 8 4 37 6 Medicine Radiology & Pathology Surgery Total 14 6 15 39 51 12 31 110 16 71 CLINICAL SERVICES CONTRACTS WHS has a contractual relationship with the following Capital City-based provider groups or professional associations (PAs) for the following services. These groups also support OMC and most OHA-affiliated hospitals: Anesthesiology. DO Anesthesiology Associates PA assigns to WHS four anesthesiologists and four nurse anesthetists as well as other staff as needed. Emergency medicine. DO Emergency and Occupational Health Associates PA assigns to WHS emergency physicians on a permanent basis along with other physicians as needed. WHS augments the emergency medicine staff with physician assistants. Pathology. DO Pathology Services PA assigns to WHS physicians who perform pathology services. As needed, additional pathologists are brought in or the procedure is done at OMC. Radiology. DO Radiology Services PA assigns to WHS radiologists and provides other clinical services. This group's main office and primary service locations are electronically linked so that its radiologists - wherever they may be working-can access patient data, read and interpret scans and images, and dictate reports. DEPARTMENT OF MEDICINE This department comprises physicians in private practice whose specialties include general and family practice, internal medicine, pediatrics, cardiology, and ENT (ear, nose, throat). Dr. Paul Tafy is the elected chair of the Department of Medicine. DEPARTMENT OF SURGERY This department comprises physicians in private practice whose specialties include general surgery, OB/GYN (obstetrics and gynecology), and orthopedic surgery. Dr. Doris Felix is the elected chair of the Department of Surgery. SUBSIDIARY ORGANIZATIONS Webster Affiliate, Inc. This tax-paying PHO engages in projects of mutual interest to both WHS and members of its medical staff who are in private practice. WHS owns 70 percent of the Webster Affiliate stock and thus appoints two of the PHO's three board members. Currently, Webster Affiliate owns a number of medical offices and leases the facilities to the physicians for a fee. Webster Physicians, Inc. Owned solely by WHS, Webster Physicians is a tax-paying corporation that owns or operates medical practices for physicians affiliated with WHS. In addition, it provides contractual management services, such as information technology, maintenance, and billing - to other medical practices. MEDICAL STAFF ORGANIZATION Dr. George Taff (Department of Medicine) has been president of the medical staff for the past three years. The president is elected every two years and provided with a small stipend by WHS. Dr. Meagan Lincoln (Department of Pathology) is the vice president, and Dr. Charles Stein (Department of Surgery) is the secretary. The standing committees of the medical staff are utilization review and quality assurance, medical records, credentials, tissue, pharmacy and therapeutics, and executive. Composed of the chairs of each standing committee and each department, the medical staff's executive committee meets monthly or as needed. The other committees also meet monthly. The entire medical staff meets quarterly. At its annual meeting, the medical staff votes on recredentialing. In an interview with select members of the medical staff, Dr. Taff called the relationship among members of the medical staff "very professional" and noted that some of the older physicians seem uncomfortable with the speed but not the substance of many of the changes the medical staff and the hospital have rolled out over the years. Asked about the relationship between WHS and the physicians, he stated, Collaboratively, the hospital has assisted us with expanding our reach to young, well-trained primary care doctors and with building appropriate referral bridges to OMC. Physicians feel included in the processes and decisions in this hospital, including its strategic planning. Many have been here for decades." Dr. Taff shared that being president feels like a full-time job and that without the stipend he would be unable to meet many of its expectations. Still, he is on board to help WHS achieve its priorities. "The hospital has to continue to build up its primary care network, even if this means building offices and hiring more doctors. That should be a priority," he said. The immediate priority of the PHO should be medical practice management. The previous priority of installing an information system that supports both the clinical and administrative sides is now a reality. I'm very impressed with how the hospital implemented the EHR and ensured its meaningful use. We are a model within the OHA system. Medically, the hospital needs to establish a much stronger presence outside of Middleboro, although that may be hard to do in Jasper given its upcoming highway, which will take people straight to the hospitals in Capital City." Other physicians agreed with Dr. Taff. For example, Dr. Lasker, a member of the medical staff for 32 years, said, Reducing inpatient beds after years of expansion felt strange but clearly was the right thing to do. He admitted that the relationship he has with many nurses really helps him practice high-quality, cost-effective medicine. The ongoing studies for appropriate ways to shorten lengths of stay are one example of how this hospital has faced up to the challenges and responded appropriately," he said. Dr. Kelly, another longtime member of the medical staff, indicated that the hospital needs to continue to expand outpatient services and provide community Outreach to high-risk individuals, especially in the rural area to the north of the city. According to her, the medical staff fully supports WHS's acquisition of select medical practices. For those physicians, this model removes the burden of managing a practice and gives them direct access to the hospital's EHR, she explained. Dr. Able, a new member, shared that she sees great possibilities with the PHO, strongly supports the recruitment of family practice physicians from OMC (like herself), and appreciates the support WHS gives to those who want to start a thriving practice. Although my practice is located in a rural area, I do not feel isolated because of all the support I get. I still have a good relationship with many of the faculty who trained me at OMC Medical School, she added. Dr. Pelopolis, a veteran at the hospital, was the only physician who offered any critic comments, concerned that conti to be a outpost OMC. "I am most that OMC-contracted physicians-such as Dr. Lincoln-hold leadership positions on our medical staff. Our medical staff has lost the ability to chart its own course." This perspective is shared by a small number of other WHS physicians. However, they realize that if OMC physicians were ineligible for leadership positions, WHS physicians would be in their place and fewer physicians would be able to share the duties of the medicine and surgery departments, making more work for everyone. Dr. Pelopolis, however, has remained adamant about this issue and has written to physicians in these two departments to persuade them to discuss the issue at their next departmental meeting. Currently, WHS does not employ hospitalists. We take care of our own, Dr. Taff reasoned. Maybe someday we will need assistance with inpatient care, but not today. That said, he has been working on a proposal to contract with OHA for 48-hour hospitalist coverage on the weekends. WHS has taken no official position on using hospitalists. CHALLENGES AND FUTURE PLANS BEHAVIORAL HEALTH The OHA board has recommended that OHA develop one or more dedicated units in its affiliate hospitals that specialize in drug- and alcohol-addiction treatment. Once these units are operational, "at least one of the hospitals should also develop a comprehensive inpatient psychiatric facility to serve the entire OHA system," the board said. WHS is one of the affiliates the board is targeting, promising to furnish the hospital with planning parameters if it wishes to assess the feasibility of this project. WHS already has long-standing agreements with Sockalexis Center and Middleboro Community Mental Health Center to provide inpatient emergency psychiatric services, including suicide watch, to WHS patients. Under these agreements, the centers limit emergency psychiatric admissions to 48 hours before the patient must be transferred and cap the total number of inpatient days at 100 per year. OCCUPATIONAL HEALTH AND OTHER BOARD CONSIDERATIONS Eric Martin, a member of WHS's board, brought to the board's attention that Physician Care Services (PCS), Inc. may be put up for sale in the near future. According to Martin, the CEO of Carlstead Rayon, PCS provided occupational health services to his employees for many years and, in the process, helped "lower our workers' comp and occupational health costs by at least 15 percent," he said. The company, however, moved its occupational health contract to MIDCARE five years ago. In another meeting, board chair Daniel Will stated that the board would receive "briefing papers" on the following issues. He asked all members to review these materials for the next meeting's discussion: Should we review the current Affordable Care Act provisions? Should future physician recruitment emphasize primary care or specialty care? Do we need to recruit to replace specific physicians and surgeons? Should we hire a chief information officer and establish an in-house information systems department to support operations and WHS-owned or managed medical practices? What is the future of the hospital's existing consulting and service contracts that address our information systems need? Is there a need and demand for new surgical technologies? Which new technologies should we prioritize? Should the hospital establish an outpatient clinic in the northern rural communities? Where should/could this clinic be located? What services should be provided? What are the associated costs and benefits? What are the ramifications of a rumored 15 to 30 percent increase in OHA affiliation fees? Should the hospital continue its ten-year plan to earn LEED (Leadership in Energy and onmental Design) certification? PRIVATE ROOMS OHA is considering an initiative to brand all affiliated hospitals on the basis of quality and privacy. It had asked each hospital affiliate to indicate its potential bed needs for 2020 and beyond and to undertake a study to determine the financial ramification of making all inpatient medical-surgical beds private (instead of semiprivate). Existing semiprivate rooms can be modified into private rooms for approximately $425,000 per room, and new private rooms (minimum of ten) can be added for approximately $1 million per bed. (These values are expressed in 2019 dollars.) The analysis should assume a 20-year straight-line depreciation approach and no salvage values. OHA can commit up to 70 percent financing at an annual interest rate that does not exceed 4 percent. OHA POLICY CONCERN At a recent meeting of the OHA board, affiliates indicated that their supply costs per case-mix adjusted discharge were higher than they should be" and asked OHA to change its policy of requiring affiliates to secure all supplies from OHA. This topic was included on the agenda for the next meeting. POTENTIAL LEGISLATIVE CHANGE This past month, OMC alerted all affiliated hospitals (confidentially) that the Office of the Governor is working with other states on model legislation to limit statewide hospital costs. One model being considered limits annual hospital spending increases to the annual increase in the gross state product. Another option is to decrease hospital Medicaid rates by 3 percent for each of the next ebster Health System (WHS), formerly called Webster Hospital - constitutes a hospital and a for-profit organization that are jointly owned by the system and members of the medical staff. The hospital is accredited by the American Osteopathic Association and is an affiliate member of Capital City-based Osteopathic Hospitals of America, Inc. In its recent report to the American Hospital Association, the hospital indicated it employs 704 personnel; is licensed to operate 105 inpatient beds; and has met all the conditions necessary for Medicaid, Medicare, and Blue Cross insurance coverage. Currently, it staffs 85 inpatient beds and has a case-mix index of 1.2155. Table 5.1 lists the hospital's services. W HISTORY PHYSICAL STRUCTURE The original 1930s hospital was a three-floor brick structure built to accommodate 70 inpatient beds. Surrounding the facility were houses purchased by the hospital. Over the years, the building has undergone expansions and renovations. For example, in 1989, the space was reconfigured to increase the number of inpatient beds to 105, an addition that was later cut back to its current size of 85. The most recent modernization program was completed seven years ago. It installed modern features that make the hospital more attractive and rearranged spaces to make operations and care delivery more efficient. It also expanded the maternity unit so that, when possible, all maternity services, including labor and delivery-are contained in the mother's private room. The homes next to the facility have been converted into offices for the 12 members of the medical staff. All of the other land on the hospital campus remains undeveloped. The hospital and adjacent offices, each of which complies with current building standards and codes, sit on a 16-acre campus located in southeastern Middleboro next to the interstate highway. WEBSTER HOSPITAL Founded in 1930 by Dr. Edward W. Webster as a short-term, general acute care nonprofit, the hospital has had close ties with Osteopathic Medical Center (OMC) in Capital City even before Osteopathic Hospitals of America (OHA) was established. Dr. Webster was a senior osteopathic physician at OMC, and in 1929, upon arriving in Middleboro, he began a community campaign to found a hospital that would serve as an alternative to Middleboro Community Hospital. He was the first superintendent of Webster Hospital and was successful in establishing osteopathic medicine in Hillsboro County. The Webster family still financially supports WHS. In the past 20 years, his sons and grandsons have continued to increase its endowment. Since 1930, the hospital's relationship with MIDCARE,then called Middleboro Community Hospital - has been strained. Here are some examples: In 1996, Webster Hospital and Middleboro Community Hospital dissolved their more than 30-year joint venture corporation for shared laundry services. Middleboro Community Hospital elected a provision in the original 1965 agreement to buy Webster Hospital's share of the joint venture, even though Webster Hospital wished to retain the partnership. At the time of the forced sale, Middleboro Community Hospital indicated that its need for laundry services could only be met if it fully owned the laundry corporation. Middleboro Community Hospital did offer to provide laundry services to Webster Hospital on an annual contract, but Webster Hospital determined that establishing its own laundry service would be more efficient. . In 1998, Webster Hospital terminated a joint education agreement with Middleboro Community Hospital. Under this agreement, staff members of both hospitals received continuing education at both institutions. In 1999, a formal joint committee of the boards of each hospital explored the possibility of a merger of the two organizations. Although supported by both CEOs, the merger was deemed not feasible by the committee. Since that time, the two entities have had minimal contact and have been increasingly competitive with each other. . In 2000, when Webster Hospital signed the affiliation agreement with OHA and became WHS, the president and board chair of Middleboro Community Hospital published an open letter in the Middleboro Sentinel. The letter indicated these leaders' disappointment that a community hospital in Middleboro was now going to be directed by a medical center based outside of the community" in Capital City. The letter went on to say, "We wish it had been obvious to us that Webster Hospital needed help to continue its operations. We would have assisted with providing quality care at a reasonable price for our community, as we do now." Today, the sole remaining agreement between the two hospitals is compelled by regulation. Under this agreement, WHS patients and others under the care of an osteopathic doctor may come to MIDCARE for ambulatory cancer treatment. This provision was required by the state when it issued to MIDCARE the certificate of need for this service. OHA AFFILIATION Established in 1990 and headquartered in Capital City, OHA was developed to provide corporate direction and control for osteopathic hospitals in the tri-state region. It is a nonprofit corporation with a regional network currently composed of 18 affiliated organizations. These affiliates are nonprofit, community osteopathic hospitals that provide tertiary care. Each hospital elects to affiliate with the system and retains its independent corporate status. OHA has a board of directors chaired by Harry Swift. Annually, the board votes to retain an affiliate member. The board also has the ability to sever an affiliation contract with just a three-month notice. As an affiliate member of OHA, WHS is subject to OHA's affiliate program. Under this program, a hospital agrees to do the following when it signs a formal affiliation contract (renewed annually): Retain the hospital's affiliate membership for at least three years, and elect one person to the OHA board of directors. Provide consulting and/or active privileges to all qualified physicians whom OHA recommends. Record all patient care information using the OHA medical records system, and share an abstract of this information with OHA. Purchase all supply items (medical and nonmedical) and durable medical equipment through OHA. Share with OHA a draft of the hospital's revenue and expense budget for the next fiscal year, and bring to the hospital's board OHA's comments on this budget. Allow OHA the first option for purchase if the hospital decides to change its ownership status. Pay OHA an annual affiliation fee of 0.5 percent of the hospital's gross charges or $1 million, whichever is less. In return for this affiliation, a hospital receives the following services and benefits at no additional cost: Board education Development of the hospital's strategic plan and quality assurance system Access to capital for projects approved by OHA at the prime rate +0.2 percent Continuing medical education . Consulting services related to electronic health records, financial management, human resources administration, health benefit surveys, and new service development Tele-Med Services, a high-speed voice and video communications link between the attending physicians at an affiliated hospital and physicians at OMC Regional and community-specific advertising Under the affiliation agreement, a hospital may lease from OHA a CEO at cost; use OHA-marked services, such as Quick Med; and book OMC Air Evac transportation at cost. Currently, 62 percent of all osteopathic hospitals the tri-state area are affiliated with OHA. OHA is organized into three separately operated corporations: OMC, OHA Hospital Services, and OHA Ventures. OMC Located in Capital City, OMC is a nonprofit, 210-bed medical center that provides a full range of acute and tertiary care services. It is a Level I trauma center as well as a designated teaching hospital that offers approved residencies in most medical specialties. Medical interns and residents visit WHS regularly as part of their community medicine training. Five years ago, in collaboration with State University, OMC launched degree programs for physician assistants and advanced nurse practitioners, with numerous specialties for the latter. Dr. Samuel Gilbert, an osteopath, is the president of OMC. OHA HOSPITAL SERVICES, INC. This nonprofit corporation, based in Capital City, provides services to OMC and all OHA-affiliated hospitals. Currently, it offers the following services: . Retirement planning Hospital risk-management programs Health services consulting Outplacement and recruiting Capital financing Meaningful use advisory EHR and medical record systems development and support Data warehousing Pharmacy contract management OHA Hospital Services is headed by Garrett Fulerman. OHA VENTURES, INC. This Capital City for-profit is headed by Rose Flagstaff and currently specializes in managing medical groups. It also owns and operates medical office buildings. Three years ago, OHA Ventures introduced a joint purchase and management program that enables an OHA-affiliated hospital to copurchase and comanage individual medical practices with OHA Ventures. To date, no physician practice affiliated with WHS has elected to use OHA Ventures as a practice manager. In the same period as the launch of the joint program, OHA Ventures independently began purchasing orthopedic, family practice, and cardiology practices of physicians affiliated with OHA- affiliated hospitals. As a result, all of these physicians become employees of OHA Ventures and are granted consulting status at OMC. Because OHA-affiliated hospitals are, generally, not interested in purchasing and managing medical practices, OHA Ventures had to justify this program to the OHA board. Flagstaff reasoned that the purchase would relieve physicians from the burden of practice management, allowing them to practice medicine instead, and would prevent osteopathic practices from being bought by allopathic hospital systems. To date, OHA Ventures has purchased 24 medical practices and has three outstanding offers. In Hillsboro County, OHA Ventures owns three practices in Jasper: an OB/GYN practice (sold by Drs. Morton and Salt), a family practice (sold by Drs. Dadoveci, Child, Megg, Kidd, and Lady), and a pediatric practice (sold by four physicians not affiliated with WHS). One hospital in another region of the state withdrew its OHA affiliation when OHA Ventures outbid it for an orthopedic practice. Three affiliates sued OHA Ventures for breach of contract, claiming these purchases violate the affiliate contractual relationship. The case was dismissed, with the court ruling that the "affiliate contract does not prohibit OHA or its subsidiaries from purchasing medical practices, especially given that the owners of the medical practices can entertain multiple offers, including offers from the affiliate member." GOVERNANCE WHS's board of trustees is composed of eight individuals. The 100 incorporators elect trustees on the basis of nominations by the board's nominating committee. Trustees are elected for four-year terms, with the stipulation that they may serve no longer than two consecutive terms. Current board trustees of WHS are as follows; the (number)* indicates the number of years remaining on current board term, and the number)+ indicates the trustee's second term: WHS Board of Trustees Residence Middleboro Mifflenville Jasper Boalsburg Members Daniel Will (2)* +, Chair Attorney, Will & Associates Harlan Crowe (3), Vice Chair President, Farmers and Merchants Bank Yolanda Nice (4), Secretary Director of Human Resources, U.S. Parts Belinda Bond (1)+, Treasurer Retired stockbroker Eric Martin (4), At-Large President and CEO, Carlstead Rayon Tracy Meyer (2), At-Large Vice president of Finance, River Industries Samuel Mudd, DO (3), At-Large Retired physician Mike Webster (1), At-Large Proprietor, Webster Family Farm The standing committees of the board are as follows: Middleboro Middleboro Middleboro Statesville Executive (Will, Crowe, Nice, Bond) Finance (Crowe, Bond, Martin) Joint Conference (Will, Dr. Taff, Swisher) Long-Range Planning (All Trustees) Medical Manpower/Credentials (Dr. Mudd, Meyer, Webster) Nominating (Nice, Crowe, Martin) Quality Assurance (Meyer, Will, Dr. Mudd) The board meets monthly, the executive committee meets twice a month, and other committees meet as needed (usually monthly). Every December, the board-along with the hospital auxiliary - sponsors a hospital fund-raising event called Holiday Ball at the Middleboro Golf Club. MANAGEMENT TEAM AND ORGANIZATIONAL STRUCTURE PRESIDENT AND CEO Steve Swisher, CPA, was promoted to president and CEO nine months ago. Prior to this appointment, he was vice president of Administrative Services and chief financial officer (CFO) at WHS for 14 years. He holds a bachelor in accounting and a master of business administration from a midwestern university and is a member of the Healthcare Financial Management Association. Before coming to WHS, he was a senior fiscal analyst at Blue Cross and Blue Shield in Capital City. The position of president and CEO became vacant when the well-loved and respected Edith Masterman retired from the job four years ago. WHS used a national executive search firm to identify qualified candidates. The first search yielded no candidates acceptable to the board, but the second search resulted in the hiring of Stella MacArthur. Twelve months later, however, she reached a mutual agreement with the board and resigned from the post. The board offered no reason for her immediate departure. During another lengthy search, Swisher was appointed acting president. When interviewed, Swisher noted the board's concerns regarding changing market dynamics, especially in Jasper; the need to recruit new physicians for WHS's primary markets; the potential addition of specialized services; the system's financial challenges; and the development of a regional accountable care organization. He offered a "that's confidential in response to reports that WHS's affiliation with OHA has become difficult, but he said this to clear up other rumors: "Our strength is our people, who are highly skilled and dedicated to our mission. We focus on keeping them happy, so I'm not aware of any behind-the-scenes union activity among our clerical and administrative staff. In regards to the turmoil associated with my office, there's none-no turmoil. We stumbled a few times during the recruitment process, but I think that may be due to our inexperience. Edith was so good at this job for so long that we relied too much on her instead of developing our own competencies and ensuring our policies match our changing needs. For example, we don't have an experienced governing board. That's because our bylaws dictate we remove the experienced trustees after serving only two terms on the board, so we lose the organizational knowledge and insights they gained during their tenure. That holds us back, and we have to address that and other issues if we want to create a strong vision and strategies for the future." VICE PRESIDENT OF ADMINISTRATIVE SERVICES AND CFO June Taylor, CPA, replaced Swisher in this position. She was promoted from the position of deputy chief fiscal officer, where she had been for ten years. She holds a bachelor in accounting and a master of business administration from State University and is a member of the Healthcare Financial Management Association. As Swisher's direct report, she has extensive responsibilities, including overseeing these departments: Admitting, Business Office, Central Supply, Housekeeping, Laundry, Maintenance, Medical Records, Personnel, Purchasing, Security, and Telecommunications. In addition, Taylor is in charge of a laundry service contract between WHS and Hillsboro County Health Department. Several years ago, when WHS began searching for clients to use its excess laundry capacity (caused by the decrease in inpatient days), Taylor developed a contractual program that has WHS providing laundry services to Manorhaven, the long-term care facility owned and operated by Hillsboro County Health Department. She indicated that this contract, aside from being good business, keeps the hospital's laundry service an efficient operation with its current level of staffing. Another one of her many duties is as chief personnel officer, which has become an almost full-time job." She said, Our HR staff have had a hard time filling openings because there seems to be a lack of qualified, acceptable professionals in our area. We're working hard to attract them." Although Taylor remains optimistic about the future, she has worries. The hospital's inpatient capacity has gotten about as small as it should," she said. "Too much smaller, and it will become less efficient." As a result, she advocates a competitive strategy to capture ambulatory and inpatient market share historically served by MIDCARE. The good news is the hospital has a win-win relationship with the staff, including the medical staff. They know our needs, we know theirs, and we are committed to joint success," she added. Five years ago, WHS installed an electronic health record system, with full support from OHA. All medical practices owned by WHS-through Webster Physicians are connected to the system, while other affiliated practices can access the system by purchasing or leasing the software from WHS or OHA and then logging in through an online portal. Technical oversight of the system is provided by a private contractor and OHA Hospital Services. Taylor does not think the hospital needs a chief information systems officer at this time: Our current arrangement with OHA for consulting services seems to be working well. We have their expertise, and the contractor is very responsive to our needs." VICE PRESIDENT OF PROFESSIONAL SERVICES Ellen Wilgus has been employed by WHS for 15 years and was director of Physical Therapy right before her appointment as vice president. She holds a bachelor in physical therapy from State University. She has served as president of the state chapter of the American Physical Therapy Association and remains active in professional organizations related to physical therapy and rehabilitation Wilgus reports to the president and has responsibility for the following departments: Anesthesiology, Dietary, Laboratory, Pharmacy, Physical Therapy, Radiology, Respiratory Therapy, and Social Services. The ever-increasing complexity of hospital management and the greater competition from MIDCARE are among her top concerns; she thinks WHS faces an uncertain future, even with its affiliation with OHA. The hospital's decision to retain extra staff, and retrain them when needed, as it changes its primary orientation away from inpatient services made all the difference in the world, she explained. Staff became creative problem solvers because they knew they were not going to lose their jobs. She also indicated feeling supported by her hardworking department heads and especially proud that the most recent accreditation review found no significant deficiencies in any of the departments she oversees. Years ago, Wilgus headed the management task force that implemented the maternity unit redesign and expansion. For her exemplary performance on the task force, she earned an official commendation from the medical staff as well as a special recognition from the board and the former president. Currently, she leads the continuous quality improvement team's effort to shorten the length of inpatient hospital stays per diagnosis-related group. VICE PRESIDENT OF CLINICAL SERVICES Gretta Schmidt, RN, was hired to replace a retiring vice president. Prior to coming to WHS, she held numerous nursing positions at MIDCARE, including associate director of nursing, making her the first senior management member to have worked for a direct competitor; her selection was a unanimous decision approved by leadership. She graduated from MIDCARE School of Nursing, has a bachelor and master in nursing from State University, and is active in the state nursing association. Like the other vice presidents, Schmidt reports to the president and is in charge of multiple departments, including Clinical Education, Pediatrics, Intensive Care, Medical Surgical Unit I, Medical Surgical Unit II, Medical Surgical Unit III, Emergency and Outpatient Departments, and Staff Development. WHS maintains a high nurse-patient ratio and is making progress in achieving an all-RN (registered nurse) nursing staff, something she is concentrating on. When interviewed, Schmidt was careful with her remarks about MIDCARE, stating, I'm unsure about the real issues between MIDCARE and this hospital. I sure am very impressed, though, by the high clinical competence of the nursing staff here. Nurse turnover is not as big an issue here as it is at MIDCARE. She is equally complimentary of the professional relationship between physicians and nurses. Although there is no formal joint practice program, most aspects of joint practice characterize the nurse-physician relationship, she said. VICE PRESIDENT OF MARKETING David Story, who is from a prominent family in Middleboro, has been the marketing head at WHS for 12 years and, before that was deputy director of marketing for a durable medical equipment firm in Capital City. He holds a liberal arts degree and a master of health administration from an eastern university and is a member of the American College of Healthcare Executives (ACHE). His tenure at WHS has been productive from the beginning, and these successes have not been limited to marketing. He secured the certificate of need for the hospital's first CT (computed tomography) scanner. He recruited a number of physicians, many of whom are still on the medical staff. He, along with Swisher, negotiated a long-term financial loan with OMC to finance a project. Currently, he is working with Schmidt and the medical staff to examine the feasibility of establishing a women's health center at WHS. He also serves as the director of Webster Affiliate, Inc., the physician-hospital organization (PHO) he created to facilitate joint ventures - including joint medical practices-between the hospital and members of the medical staff. MANAGEMENT INTERN This advisory staff position is currently held by Justin Perkins, who recently earned a master of business and hospital administration from an eastern university and is completing a 24-month postgraduate fellowship program recognized by ACHE. Under the terms of this fellowship, the hospital has made no long-term employment commitment to him. A son of an osteopathic physician, Perkins was a unit manager at a large medical center before entering graduate school. Currently, he provides staff support to the president as well as to several board and hospital committees and has been managing WHS's Employee of the Month/Year program. He is a member of ACHE. INTERNAL REVENUE SERVICE FORM 990 DISCLOSURE According to WHS's recent IRS Form 990, the following are the ten highest-paid hospital employees: Staff Name Position Current Salary($) Steve Swisher President/CEO 328,500 June Taylor CFO 303,000 Gretta Schmidt, RN VP, Clinical Services 208,000 Jay Jill, RN Associate VP, Clinical Services 162,040 Carla Fox Associate VP, Administration 110,340 Ellen Wilgus VP, Professional Services 105,370 Heidi Watkins Associate VP, Finance 105,230 David Story VP, Marketing 104,220 David Crow Laboratory Director 94,500 Marvin Gardens Pharmacy Director 93,440 Total compensation includes benefits, which are 40 percent above salary. The hospital does not directly employ any physicians in these specialties: emergency, radiology, pathology, and anesthesiology. These services are provided by contracted professional associations. MEDICAL STAFF AND MEDICAL RESOURCES Currently, the WHS medical staff has 110 physicians. All physicians are graduates of osteopathic schools of medicine and have completed internships and residencies in their respective areas of expertise. All active and consulting physicians must be board certified, unless this requirement is formally waived by the executive committee of the medical staff. See Table 5.2 for a full list of WHS's medical staff. On the web at ache.org/books/Middleboro2 All consulting physicians are required to maintain active status on the medical staff of OMC in Capital City or another accredited hospital. At WHS, the majority of the active medical staff provides primary care. Patients who need higher-level procedures, tests, and medical interventions are referred or transferred to OMC or are served by consulting members of the OMC medical staff (who travel to WHS when needed). WHS maintains a helicopter landing pad on its roof to allow the rapid transfer of emergency patients to OMC using the OMC Air Evac transportation service. OMC Air Evac is also used to fly consulting physicians from OMC to WHS in an emergency. Air travel time from WHS to OMCand vice versais approximately 26 minutes. When weather conditions do not permit air transfer, patients are moved in an ambulance to OMC or MIDCARE. Following is a breakdown of the medical staff composition: Services/Department Active Physicians Consulting Physicians Total Anesthesiology Emergency 12 4 0 4 8 4 37 6 Medicine Radiology & Pathology Surgery Total 14 6 15 39 51 12 31 110 16 71 CLINICAL SERVICES CONTRACTS WHS has a contractual relationship with the following Capital City-based provider groups or professional associations (PAs) for the following services. These groups also support OMC and most OHA-affiliated hospitals: Anesthesiology. DO Anesthesiology Associates PA assigns to WHS four anesthesiologists and four nurse anesthetists as well as other staff as needed. Emergency medicine. DO Emergency and Occupational Health Associates PA assigns to WHS emergency physicians on a permanent basis along with other physicians as needed. WHS augments the emergency medicine staff with physician assistants. Pathology. DO Pathology Services PA assigns to WHS physicians who perform pathology services. As needed, additional pathologists are brought in or the procedure is done at OMC. Radiology. DO Radiology Services PA assigns to WHS