Question: I included the PBS article for reference! Assignment for Discussion Board #2: Read the information contained in the two links provided in this week's folder
I included the PBS article for reference!
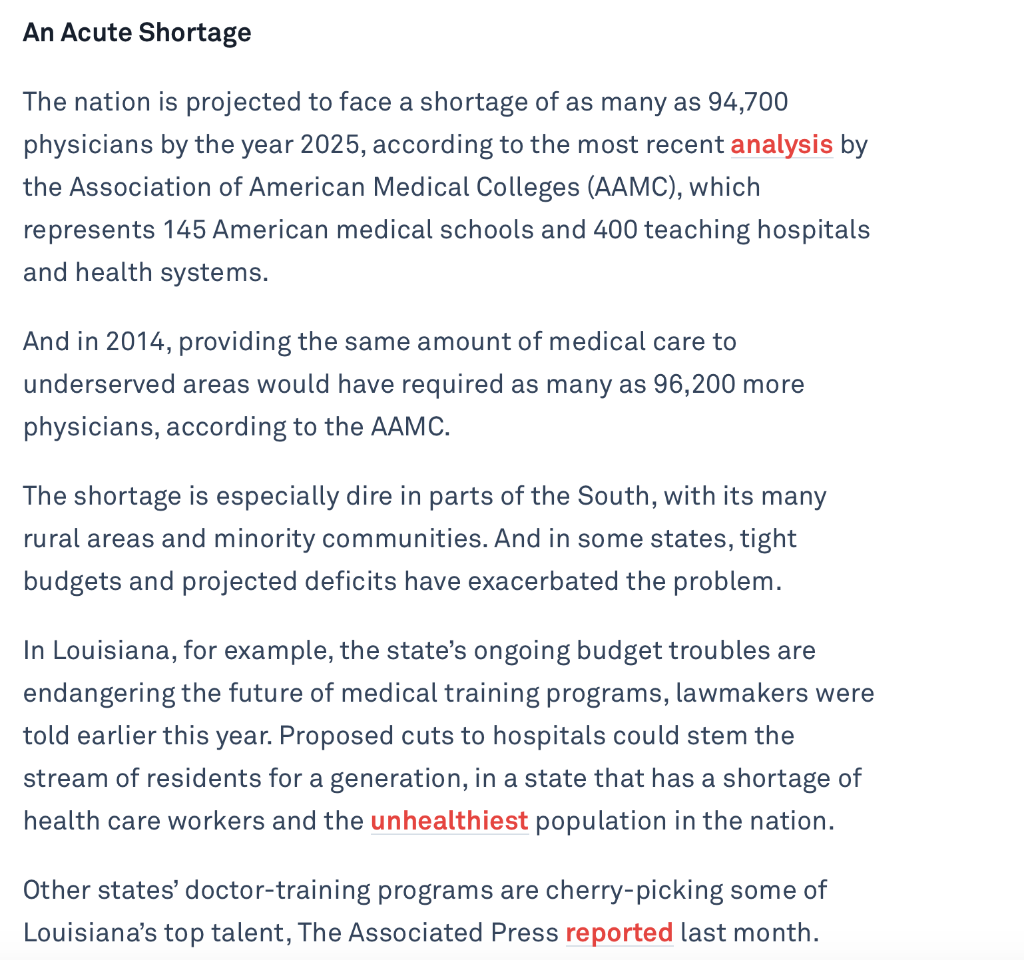
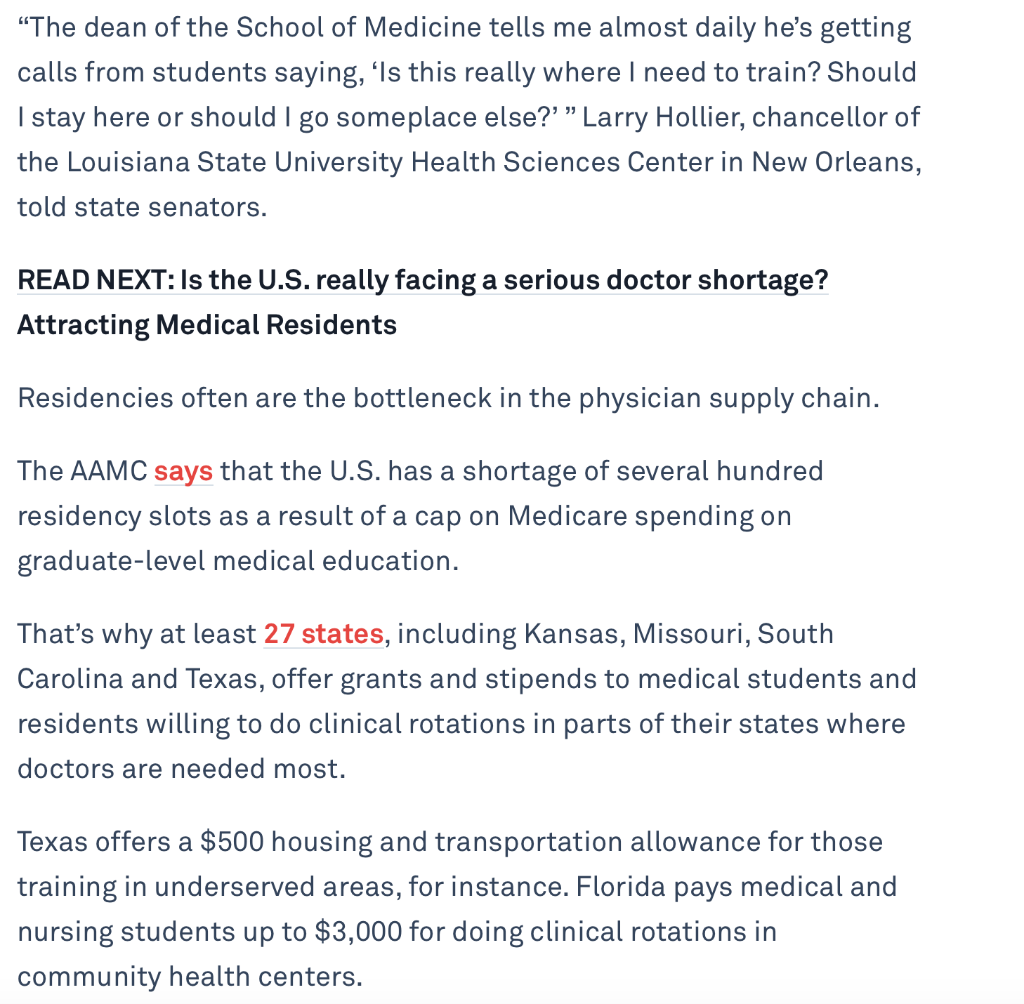
Assignment for Discussion Board #2: Read the information contained in the two links provided in this week's folder (Week 7). Answer the following 2 sets of questions; each Question has multiple parts. Your initial responses are due by 11:59 pm on Friday October 9, 2020. . Question #2: View the two PBS links in the Week 7 folder. Then answer the following questions: (Your answers must come from the PBS Links). What are two reasons students might turn away from becoming doctors in the U.S.? What are two ways in which hospitals are coping with the lack of doctors, mainly primary care physicians? Why is this information important to us as public health professionals now and in the future? . An Acute Shortage The nation is projected to face a shortage of as many as 94,700 physicians by the year 2025, according to the most recent analysis by the Association of American Medical Colleges (AAMC), which represents 145 American medical schools and 400 teaching hospitals and health systems. And in 2014, providing the same amount of medical care to underserved areas would have required as many as 96,200 more physicians, according to the AAMC. The shortage is especially dire in parts of the South, with its many rural areas and minority communities. And in some states, tight budgets and projected deficits have exacerbated the problem. In Louisiana, for example, the state's ongoing budget troubles are endangering the future of medical training programs, lawmakers were told earlier this year. Proposed cuts to hospitals could stem the stream of residents for a generation, in a state that has a shortage of health care workers and the unhealthiest population in the nation. Other states' doctor-training programs are cherry-picking some of Louisiana's top talent, The Associated Press reported last month. "The dean of the School of Medicine tells me almost daily he's getting calls from students saying, Is this really where I need to train? Should I stay here or should I go someplace else?' Larry Hollier, chancellor of the Louisiana State University Health Sciences Center in New Orleans, told state senators. READ NEXT: Is the U.S.really facing a serious doctor shortage? Attracting Medical Residents Residencies often are the bottleneck in the physician supply chain. The AAMC says that the U.S. has a shortage of several hundred residency slots as a result of a cap on Medicare spending on graduate-level medical education. That's why at least 27 states, including Kansas, Missouri, South Carolina and Texas, offer grants and stipends to medical students and residents willing to do clinical rotations in parts of their states where doctors are needed most. Texas offers a $500 housing and transportation allowance for those training in underserved areas, for instance. Florida pays medical and nursing students up to $3,000 for doing clinical rotations in community health centers. But other state efforts to provide medical care in underserved areas have been met with opposition. The AAMC, the American Medical Association and the American Association of Colleges of Osteopathic Medicine opposed the new laws allowing medical school graduates in Arkansas, Kansas and Missouri to treat patients before finishing their residencies. They argued that medical school alone doesn't prepare a physician to begin practicing. For that, they said, graduates still need clinical residency training. More Schools, More Students The solution to the shortage is producing more doctors, and the nation doing so gradually. The AAMC says medical school enrollment nearly 87,000 has increased 25 percent since 2002. The increase is even more pronounced when it comes to doctors practicing osteopathic medicine, who are trained in separate medical schools and treat patients more through touch and physical manipulation. Since 2002, the number of students enrolled in osteopathic medical school has more than doubled, to nearly 26,000, according to the American Association of Osteopathic Medicine. Osteopathic medical schools also have a tradition of locating in underserved areas. And as the new partnership in Arkansas shows, they will branch out into other states, often in association with existing universities. The Edward Via College of Osteopathic Medicine (VCOM), a nonprofit, opened its first campus in 2002 on the campus of Virginia Tech University, in southwestern Virginia. At the time, all three of the state's medical schools were in the eastern part of the state. State officials and those at Virginia Tech concluded that the VCOM campus would be the best way to address the severe doctor shortage in that part of the state. In recent years, VCOM opened new branches in South Carolina, in partnership with Wofford College, and in Alabama, with Auburn University as its partner. This fall, the nonprofit Burrell College of Osteopathic Medicine will welcome its first class on the campus of New Mexico State University. The hope is that the school will bring doctors to underserved southern New Mexico. The new partnership in Arkansas, between the public university and the private medical school, grew out of talks on how to bring more primary care doctors to the rural and poor Delta region of the state. Rather than start its own costly medical school, Arkansas State University concluded in 2013 that attracting a branch of an osteopathic school would be best because of osteopathic medicine's emphasis on primary care and because its schools do not require large research facilities that are expensive to maintain. The medical school will lease the historic, centrally located Wilson Hall on the university's campus for about $300,000 a year. Renovations cost $12.6 million, with each school contributing $2.3 million up front. Arkansas State University borrowed to cover the rest of the costs, which is expected to be paid back from rent paid by the medical school. Jason Penry, the university vice chancellor, said the new school will recruit students heavily from Arkansas to increase the chances that graduates will remain to practice in the state. Jason Penry, the university vice chancellor, said the new school will recruit students heavily from Arkansas to increase the chances that graduates will remain to practice in the state. Medical school students will have the same access to the university's libraries, gyms and other facilities as other students. And the medical school will be equipped with technology so that students on the Long Island and Jonesboro campuses can attend lectures at the other. In a resource-short environment this was a way of bringing decades of experience in medical education to the state and region in need," Penry said. offer health benefits, giving rise can afford it and welfare services concern about a "dactor . 19003 1910s 1920s 19309 1940s 1950s 1960s Consistent with the general American Medical Association American hospitals are now The Depression changes At the start of the decade, Penicillin comes into use. In the 1950s, the price of (AMA) becomes a powerful modern scientific Institutions, mood of political complacency, priorities, with greater emphasis national health care expenditures hospital care doubled. Now in the national force. valuing antiseptics and there is no strong effort to on unemployment insurance and early 1960s, those outside the cleanliness, and using change health insurance, "old age" benefits. medications for the relief of pain. Reformers now emphasize the Prepaid group healthcare begins, are 4.5 percent of the Gross workplace, especially the elderly, In 1901, AMA reorganizes as the have difficulty affording Social Security Act is passed, Attention turns to Korea and Insurance. national organization of state and cost of medical care instead of omitting health insurance. During the 2nd World War, wage away from health reform local associations. Membership wages lost to sickness - the American Association for Labor and price controls are placed on America will have a system of increases from about 8,000 Over 700 insurance companies Legislation (AALL) organizes first relatively higher cost of medical Push for health insurance within American employers. To compete private insurance for those who physicians in 1900 to 70,000 in selling health insurance. national conference on "social care is a new and dramatic 1910 -- half the physicians in the the Roosevelt Administration, but for workers, companies begin to development, especially for the , insurance". politics begins to be influenced country. This period is the . middle class. by internal government conflicts to the employer-based system in for the poor. beginning of organized shortage" and the need for more place today. over priorities. Progressive reformers argue for medicine." Federal responsibility for the sick "health manpower" leads to health insurance, seems to be Growing cultural Influence of the President Roosevelt asks poor is firmly established, federal measures to expand medical profession - physicians' Against the advice of insurance gaining support. Surgery is now common, education in the health incomes are higher and prestige professionals, Blue Cross begins Congress for economic bill of Many legislative proposals are professions. especially for removing tumors, is established. Opposition from physicians and infected tonsils, appendectomies, other interest groups, and the offering private coverage for rights,"Including right to made for different approaches to adequate medical care. hospital care in dozens of states. hospital Insurance, but none Major medical Insurance and gynecological operations. Rural health facilities are clearly entry of the US into the war in endorses high-cost medicine. President Truman offers national succeed. 1917 undermine reform effort. inadequate. Doctors are no longer expected health program plan, proposing a to provide free services to all President Lyndon Johnson signs General Motors signs a contract single system that would include Many more medications are Medicare and Medicaid into law. hospital patients. with Metropolitan Life to insure available now to treat a range of all of American society. 180,000 workers. diseases, including infections, America lags behind European Truman's plan is denounced by glaucoma, and arthritis, and new "Compulsory Health Insurance" advocates are no longer countries in finding value in the American Medical Association vaccines become available that Penicillin is discovered, but it will insuring against the costs of CAMA), and is called a optimistic. prevent dreaded childhood sickness. be twenty years before it is used Communist plot by a House diseases, including polio. The to combat infection and disease. subcommittee first successful organ transplant The number of doctors reporting themselves as full-time is performed.. Railroads are the leading industry to develop extensive employee specialists grows from 55% in 1960 to 69%. medical 1970s 1980s 1990s 2000s President Richard Nixon renames prepaid group health care plans as health maintenance organizations (HMOs), with legislation that provides federal endorsement, certification, and assistance. Corporations begin to integrate the hospital system (previously a decentralized structure), enter many other healthcare-related businesses, and consolidate control. Overall, there is a shift toward privatization and corporatization of healthcare. Under President Reagan, Medicare shifts to payment by diagnosis (DRG) instead of by treatment. Private plans quickly follow suit. Healthcare costs are escalating rapidly, partially due to unexpectedly high Medicare expenditures, rapid inflation in the economy, expansion of hospital expenses and profits, and changes in medical care including ter use of technology, medications, and conservative approaches to treatment. American medicine is now seen as in crisis. Health care costs rise at double Health care costs are on the rise the rate of inflation. again. Expansion of managed care helps Medicare is viewed by some as to moderate increases in health unsustainable under the present care costs. structure and must be "rescued". Federal health care reform Changing demographics of the legislation fails again to pass in the U.S. Congress. workplace lead many to believe the employer-based system of insurance can't last. By the end of the decade there are 44 million Americans, 16 % Human Genome Project to of the nation, with no health identify all of the more than insurance at all. 100,000 genes in human DNA is Human Genome Project to ected to be completed a full identify all of the more than two years ahead of schedule, in 2003. 100,000 genes in human DNA gets underway. Direct-to-consumer advertising for pharmaceuticals and medical By June 1990, 139,765 people in devices is on the rise. the United States have HIV/AIDS, with a 60 percent mortality rate. . Growing complaints by insurance companies that the traditional fee-for-service method of payment to doctors is being exploited. "Capitation" payments to doctors become more common. President Nixon's plan for national health insurance rejected by liberals & labor unions, but his "War on Cancer" centralizes research at the NIH. The number of women entering the medical profession rises dramatically. In 1970, 9% of medical students are women; by the end of the decade, the proportion exceeds 25%. World Health Organization declares smallpox eradicated. Assignment for Discussion Board #2: Read the information contained in the two links provided in this week's folder (Week 7). Answer the following 2 sets of questions; each Question has multiple parts. Your initial responses are due by 11:59 pm on Friday October 9, 2020. . Question #2: View the two PBS links in the Week 7 folder. Then answer the following questions: (Your answers must come from the PBS Links). What are two reasons students might turn away from becoming doctors in the U.S.? What are two ways in which hospitals are coping with the lack of doctors, mainly primary care physicians? Why is this information important to us as public health professionals now and in the future? . An Acute Shortage The nation is projected to face a shortage of as many as 94,700 physicians by the year 2025, according to the most recent analysis by the Association of American Medical Colleges (AAMC), which represents 145 American medical schools and 400 teaching hospitals and health systems. And in 2014, providing the same amount of medical care to underserved areas would have required as many as 96,200 more physicians, according to the AAMC. The shortage is especially dire in parts of the South, with its many rural areas and minority communities. And in some states, tight budgets and projected deficits have exacerbated the problem. In Louisiana, for example, the state's ongoing budget troubles are endangering the future of medical training programs, lawmakers were told earlier this year. Proposed cuts to hospitals could stem the stream of residents for a generation, in a state that has a shortage of health care workers and the unhealthiest population in the nation. Other states' doctor-training programs are cherry-picking some of Louisiana's top talent, The Associated Press reported last month. "The dean of the School of Medicine tells me almost daily he's getting calls from students saying, Is this really where I need to train? Should I stay here or should I go someplace else?' Larry Hollier, chancellor of the Louisiana State University Health Sciences Center in New Orleans, told state senators. READ NEXT: Is the U.S.really facing a serious doctor shortage? Attracting Medical Residents Residencies often are the bottleneck in the physician supply chain. The AAMC says that the U.S. has a shortage of several hundred residency slots as a result of a cap on Medicare spending on graduate-level medical education. That's why at least 27 states, including Kansas, Missouri, South Carolina and Texas, offer grants and stipends to medical students and residents willing to do clinical rotations in parts of their states where doctors are needed most. Texas offers a $500 housing and transportation allowance for those training in underserved areas, for instance. Florida pays medical and nursing students up to $3,000 for doing clinical rotations in community health centers. But other state efforts to provide medical care in underserved areas have been met with opposition. The AAMC, the American Medical Association and the American Association of Colleges of Osteopathic Medicine opposed the new laws allowing medical school graduates in Arkansas, Kansas and Missouri to treat patients before finishing their residencies. They argued that medical school alone doesn't prepare a physician to begin practicing. For that, they said, graduates still need clinical residency training. More Schools, More Students The solution to the shortage is producing more doctors, and the nation doing so gradually. The AAMC says medical school enrollment nearly 87,000 has increased 25 percent since 2002. The increase is even more pronounced when it comes to doctors practicing osteopathic medicine, who are trained in separate medical schools and treat patients more through touch and physical manipulation. Since 2002, the number of students enrolled in osteopathic medical school has more than doubled, to nearly 26,000, according to the American Association of Osteopathic Medicine. Osteopathic medical schools also have a tradition of locating in underserved areas. And as the new partnership in Arkansas shows, they will branch out into other states, often in association with existing universities. The Edward Via College of Osteopathic Medicine (VCOM), a nonprofit, opened its first campus in 2002 on the campus of Virginia Tech University, in southwestern Virginia. At the time, all three of the state's medical schools were in the eastern part of the state. State officials and those at Virginia Tech concluded that the VCOM campus would be the best way to address the severe doctor shortage in that part of the state. In recent years, VCOM opened new branches in South Carolina, in partnership with Wofford College, and in Alabama, with Auburn University as its partner. This fall, the nonprofit Burrell College of Osteopathic Medicine will welcome its first class on the campus of New Mexico State University. The hope is that the school will bring doctors to underserved southern New Mexico. The new partnership in Arkansas, between the public university and the private medical school, grew out of talks on how to bring more primary care doctors to the rural and poor Delta region of the state. Rather than start its own costly medical school, Arkansas State University concluded in 2013 that attracting a branch of an osteopathic school would be best because of osteopathic medicine's emphasis on primary care and because its schools do not require large research facilities that are expensive to maintain. The medical school will lease the historic, centrally located Wilson Hall on the university's campus for about $300,000 a year. Renovations cost $12.6 million, with each school contributing $2.3 million up front. Arkansas State University borrowed to cover the rest of the costs, which is expected to be paid back from rent paid by the medical school. Jason Penry, the university vice chancellor, said the new school will recruit students heavily from Arkansas to increase the chances that graduates will remain to practice in the state. Jason Penry, the university vice chancellor, said the new school will recruit students heavily from Arkansas to increase the chances that graduates will remain to practice in the state. Medical school students will have the same access to the university's libraries, gyms and other facilities as other students. And the medical school will be equipped with technology so that students on the Long Island and Jonesboro campuses can attend lectures at the other. In a resource-short environment this was a way of bringing decades of experience in medical education to the state and region in need," Penry said. offer health benefits, giving rise can afford it and welfare services concern about a "dactor . 19003 1910s 1920s 19309 1940s 1950s 1960s Consistent with the general American Medical Association American hospitals are now The Depression changes At the start of the decade, Penicillin comes into use. In the 1950s, the price of (AMA) becomes a powerful modern scientific Institutions, mood of political complacency, priorities, with greater emphasis national health care expenditures hospital care doubled. Now in the national force. valuing antiseptics and there is no strong effort to on unemployment insurance and early 1960s, those outside the cleanliness, and using change health insurance, "old age" benefits. medications for the relief of pain. Reformers now emphasize the Prepaid group healthcare begins, are 4.5 percent of the Gross workplace, especially the elderly, In 1901, AMA reorganizes as the have difficulty affording Social Security Act is passed, Attention turns to Korea and Insurance. national organization of state and cost of medical care instead of omitting health insurance. During the 2nd World War, wage away from health reform local associations. Membership wages lost to sickness - the American Association for Labor and price controls are placed on America will have a system of increases from about 8,000 Over 700 insurance companies Legislation (AALL) organizes first relatively higher cost of medical Push for health insurance within American employers. To compete private insurance for those who physicians in 1900 to 70,000 in selling health insurance. national conference on "social care is a new and dramatic 1910 -- half the physicians in the the Roosevelt Administration, but for workers, companies begin to development, especially for the , insurance". politics begins to be influenced country. This period is the . middle class. by internal government conflicts to the employer-based system in for the poor. beginning of organized shortage" and the need for more place today. over priorities. Progressive reformers argue for medicine." Federal responsibility for the sick "health manpower" leads to health insurance, seems to be Growing cultural Influence of the President Roosevelt asks poor is firmly established, federal measures to expand medical profession - physicians' Against the advice of insurance gaining support. Surgery is now common, education in the health incomes are higher and prestige professionals, Blue Cross begins Congress for economic bill of Many legislative proposals are professions. especially for removing tumors, is established. Opposition from physicians and infected tonsils, appendectomies, other interest groups, and the offering private coverage for rights,"Including right to made for different approaches to adequate medical care. hospital care in dozens of states. hospital Insurance, but none Major medical Insurance and gynecological operations. Rural health facilities are clearly entry of the US into the war in endorses high-cost medicine. President Truman offers national succeed. 1917 undermine reform effort. inadequate. Doctors are no longer expected health program plan, proposing a to provide free services to all President Lyndon Johnson signs General Motors signs a contract single system that would include Many more medications are Medicare and Medicaid into law. hospital patients. with Metropolitan Life to insure available now to treat a range of all of American society. 180,000 workers. diseases, including infections, America lags behind European Truman's plan is denounced by glaucoma, and arthritis, and new "Compulsory Health Insurance" advocates are no longer countries in finding value in the American Medical Association vaccines become available that Penicillin is discovered, but it will insuring against the costs of CAMA), and is called a optimistic. prevent dreaded childhood sickness. be twenty years before it is used Communist plot by a House diseases, including polio. The to combat infection and disease. subcommittee first successful organ transplant The number of doctors reporting themselves as full-time is performed.. Railroads are the leading industry to develop extensive employee specialists grows from 55% in 1960 to 69%. medical 1970s 1980s 1990s 2000s President Richard Nixon renames prepaid group health care plans as health maintenance organizations (HMOs), with legislation that provides federal endorsement, certification, and assistance. Corporations begin to integrate the hospital system (previously a decentralized structure), enter many other healthcare-related businesses, and consolidate control. Overall, there is a shift toward privatization and corporatization of healthcare. Under President Reagan, Medicare shifts to payment by diagnosis (DRG) instead of by treatment. Private plans quickly follow suit. Healthcare costs are escalating rapidly, partially due to unexpectedly high Medicare expenditures, rapid inflation in the economy, expansion of hospital expenses and profits, and changes in medical care including ter use of technology, medications, and conservative approaches to treatment. American medicine is now seen as in crisis. Health care costs rise at double Health care costs are on the rise the rate of inflation. again. Expansion of managed care helps Medicare is viewed by some as to moderate increases in health unsustainable under the present care costs. structure and must be "rescued". Federal health care reform Changing demographics of the legislation fails again to pass in the U.S. Congress. workplace lead many to believe the employer-based system of insurance can't last. By the end of the decade there are 44 million Americans, 16 % Human Genome Project to of the nation, with no health identify all of the more than insurance at all. 100,000 genes in human DNA is Human Genome Project to ected to be completed a full identify all of the more than two years ahead of schedule, in 2003. 100,000 genes in human DNA gets underway. Direct-to-consumer advertising for pharmaceuticals and medical By June 1990, 139,765 people in devices is on the rise. the United States have HIV/AIDS, with a 60 percent mortality rate. . Growing complaints by insurance companies that the traditional fee-for-service method of payment to doctors is being exploited. "Capitation" payments to doctors become more common. President Nixon's plan for national health insurance rejected by liberals & labor unions, but his "War on Cancer" centralizes research at the NIH. The number of women entering the medical profession rises dramatically. In 1970, 9% of medical students are women; by the end of the decade, the proportion exceeds 25%. World Health Organization declares smallpox eradicatedStep by Step Solution
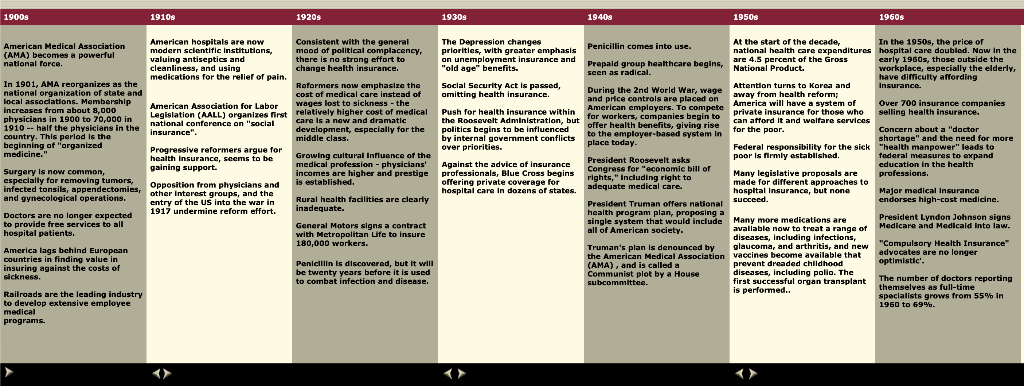
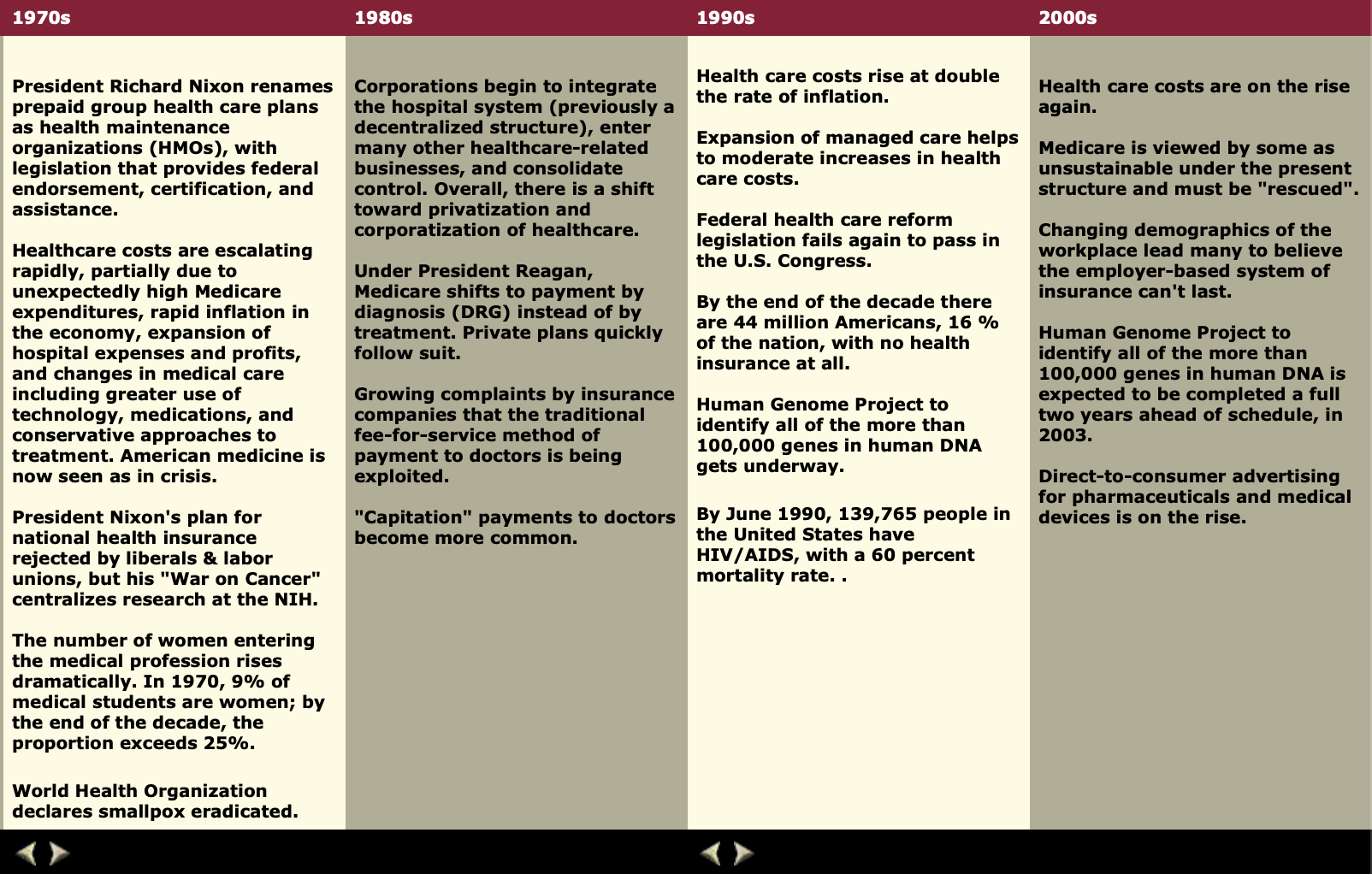
There are 3 Steps involved in it
1 Expert Approved Answer
Step: 1 Unlock


Question Has Been Solved by an Expert!
Get step-by-step solutions from verified subject matter experts
Step: 2 Unlock
Step: 3 Unlock


