Question: Please complete the Internal Analysis attached at the end **USE ONLY THIS CASE STUDY. THE GRAPHS ARE ATTACHED BELOW. THIS IS ALL THE REFERENCE YOU
Please complete the Internal Analysis attached at the end
**USE ONLY THIS CASE STUDY. THE GRAPHS ARE ATTACHED BELOW. THIS IS ALL THE REFERENCE YOU WILL NEED TO COMPLETE THE WORKSHEET, ALSO ATTACHED. THERE IS NO MISSING INFORMATION
I will be representing Christine Chassin, SVP & Chief Strategy and Business Development Officer so please fill out the form (Provided Below) as a representation of her
Christine Chassin, SVP & Chief Strategy and Business Development Officer (as told to Steve Doering)
Chassin: To my great surprise, not a single health system or physician practice group in Bay City has created an accountable care organization (ACO) in order to participate in Medicare's Shared Savings Program. Based on what Dr. Woodrow has shared with me, I think we need to investigate creating a Medicare ACO in order to prepare for the changes in health policy ahead. I recently attended the American College of Healthcare Executives conference, and accountable care was a central theme among all the presentations. It is clear to me that we must learn how to assume responsibility for the total cost of patient care. Medicare, commercial payers, and consumers understand that we cannot continue in a healthcare system where the incentives are not aligned for value. As you know, Medicare's Shared Savings Program is a program where we would create a new legal entity including a hospital, post-acute, and all required provider specialty types (CMS, 2015). This new ACO would be required to manage the total care of a group of passively assigned Medicare patients. We'd get paid a capitation rate (a per-member-per-month fee). With this money, we'd be responsible for reducing the total costs of care to below a certain benchmark set by Medicare. At the same time, we have to also meet certain quality goals. If we can do both of these things, then we get to share with Medicare in the total dollars saved. This pay-for-performance bonus could add a significant amount money to our bottom line. To take advantage of these changes, we need to leverage our computer systems that allow us to track our patients in different healthcare settings. We need to be able to look closely at the data and analyze the best ways to manage their care. I know that we have an electronic health records system already, but there are capabilities that we don't use fully. More advanced health systems have long used clinical information to better manage patients (Weaver, Ball, Kim, & Kiel, 2015). But, for us, these capabilities should be enhanced. Probably more important than technology, there are organizational capabilities that we need to improve upon in order to effectively manage care across the continuum. We have some of the best physicians in Bay City, but they can be terribly fragmented. I know there are inefficiencies in how doctors communicate with each other. I think we could pilot a more team-based approach to patient care in order to maximize efficiencies, just as we've done with the Bay City Stroke Center. I see the Medicare ACO as an opportunity to capitalize on this emerging trend in healthcare. Some of the best health systems in the country practice team-based care with great results (Goldberg, Beeson, Kuzel, Love, & Carver, 2013). It will be a real challenge to gain physician buy-in, but we can do it. As you know, I am responsible for market development at BCUHS. I see how many of our physicians are oriented toward a fee-for-service world where ordering that "extra" test is seen as financially sound. With a Medicare ACO, this culture would have to change. As I see it, it would be difficult, although not impossible, to get them to follow certain cost-saving protocols or use our electronic health records system. I think there was a pilot program at BCUHS that reduced testing amongst our medical residents. Perhaps we can build on that? Therefore, with a new ACO venture, we may have to invest in additional physician practices and lines of business, such as more primary care and post-acute care. I surmise that hospitals can lose money on these investments (Haywood & Kosel, 2011), but I believe that buying some practices and agencies in the community may be a wise long-term investment. AMCs are known for being relatively slow to adapt, less efficient than competing provider organizations, and prone to operate in ways not normal for a business operation (Grover, Slavin, & Willson, 2014). I get it. The intrinsic conflicts between an AMC's academic and business cultures are not easily reconciled. I think the time is right, though. If nothing else, we could create a first-mover advantage in managing the total care of patients.
CASE STUDY
Bay City case scenario Named the new the CEO of the nine months ago, John Woodrow, M.H.A., Ph.D. promises a new approach to strategic planning at Bay City University Health System (BCUHS). A visionary leader, Dr. Woodrow views the policy changes spawned by the Affordable Care Act (ACA) as an opportunity for BCUHS to shift from the current medical intervention model toward more holistic population health-based practices. BCUHS is an Academic Medical Center (AMC) in Bay City comprising two hospitals with more than 700 staffed beds, 150 ambulatory sites, 14,000 employees, and an operating budget of more than $2 billion. BCUHS strongly identifies with the community of Bay City, a vibrant city that serves as the metropolitan hub for more than 2 million people in the Apollo Bay region. In a recent meeting with the Strategic Planning Committee, Dr. Woodrow expressed his desire that analysts explore innovative ways for BCUHS to work across organizational boundaries, increase accountability, and improve the health of the community. Dr. Woodrow's main question was, "What will it mean for BCUHS to be held financially accountable for the total health of patients?" Dr. Woodrow explained that BCUHS needs to:
capitalize on business opportunities generated from the ACA;
improve population health management capabilities to position BCUHS to compete in light of value-based purchasing policies; respond to the emerging health care delivery models;
analyze the costs of services to take advantage of new reimbursement methods, such as capitation and global payments;
reap benefits of BCUHS's recent information technology investments; and
strengthen community connections to effectively address social determinants of health.
Strategic direction of Bay City University Health System
Steve Doering: Dr. Woodrow, thank you very much for speaking with me today. As we begin the strategic planning process, I want to get your thoughts on the strategic direction for Bay City University Health System. Do you mind if I pronounce "BCUHS" as "BECAUSE?"
Dr. John Woodrow: Not at all. I think that pronunciation reminds us that we have a sense of purpose. A "because," if you will.
Doering: Ha! That's great! So, let's get started. As you know, a strategic direction consists of three parts: mission, vision and values-all intertwined. Let's begin with our mission, our purpose and reason for existence. Can you describe what we do and for whom?
Woodrow: Absolutely. We are committed to helping all people of Apollo Bay regional area maintain healthy lives. Our mission is to eliminate health disparities in our community through service, education, and clinical practice, and scholarship.
Doering: Now, that mission helps us frame the vision, the next part of the strategic direction. The vision should describe our desired long-term future state.
Woodrow: I think the vision keeps management focused on meeting the needs of stakeholders, but we need to articulate our big stretch.
Doering: A stretch?
Woodrow: Yes. BCUHS will continue to provide care to those with the most difficult health challenges. But, with the world changing rapidly around us, I see BCUHS as a national leader in health care delivery and medical science innovation. I want to maintain our position as an education and research leader by continuing our emphasis on information technology. We can get better, though. We need to do an even better job with collaborating with our network of community and academic providers. I see us aggressively redesigning care delivery to improve care coordination. This will enable us to be a leader in population health management in our region.
Doering: That's a big vision. So, let's move on to our organizational values that define our basic philosophy, principles, and ideals. Values represent the "soul" of our organization.
Woodrow: Above all, we have to accept accountability for excellence in achieving our mission. It is not enough to say we want to eliminate health disparities in our community; we have to measure our accomplishments and adjust our performance, as appropriate. And we must advocate for equitable access to healthcare. We must respect patients and their families by providing quality care in a compassionate and culturally sensitive manner.
Doering: So how do we accomplish that?
Woodrow: We need to implement and codify the best care processes, which we call our patient-centered approach. Not only patient-centered, but evidence-based. This means that we have to create new knowledge through research, and then translate this knowledge into practice. Since we already provide the highest-quality education for the next generation of healthcare professionals, we value transferring our knowledge. Parts of our organization have already innovated care delivery through team-based care, chronic disease management, and population-based practices. Not only can we teach our organization these award-winning methods, but collaborate with others across Apollo Bay region to achieve a common purpose and create value.
Doering: Is that possible at an organization the size of BCUHS?
Woodrow: Perhaps AMCs are slow to change. However, other large and complex organizations, such as Google, are able to move quickly. I think we can innovate. Also, our brand is the one thing we value, and we must protect it. This can be done by providing exceptional performance in clinical outcomes AND patient experience. In addition, as a multifaceted healthcare system, we value lifelong care. Our brand should focus on the patient value throughout their life, and not just when they are very sick.
Doering: Is that possible at an organization the size of BCUHS?
Woodrow: Yes, but, we've got to keep cost-effectiveness in mind. "No margin, no mission," as they say. But I like to say that we have to maintain a high level of stewardship for the resources of this amazing community asset of BCUHS. So, in our everyday practice, cost efficiency should be addressed by the entire organization, with BCUHS leadership working with providers and staff to identify areas of savings.
Doering: Excellent. I think we have plenty for the teams of analysts to work with in order to create their strategic plans. Thank you.
Woodrow: Thank you.
Bay City University Health System
Overview
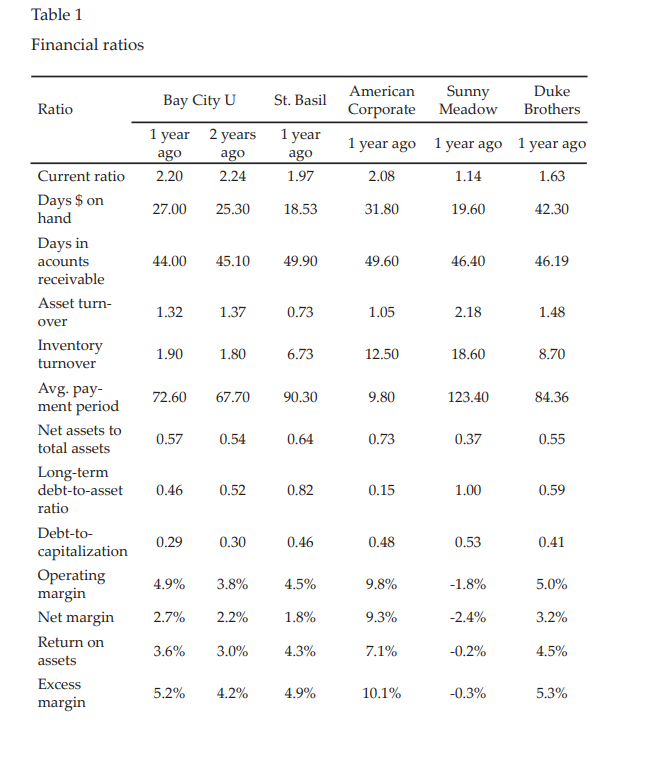
BCUHS is a nationally prominent AMC with 14,000-plus employees and an operating budget of more than $2 billion. BCUHS has a strong brand name in its geographic area, and this brand has enabled higher pricing than its competitors. However, the BCUHS also has a high-cost operating structure relative to the other institutions in the Apollo Bay region. As an AMC, BCUHS operates schools of medicine, nursing, dentistry, and public health. The BCUHS School of Medicine graduates 400 physicians each year. In addition to these students, BCUHS trains over 750 physician residents in the two hospitals, outpatient specialty clinics, and the Bay City Health Department's Neighborhood Community Health Center.
BCUHS continuum of care
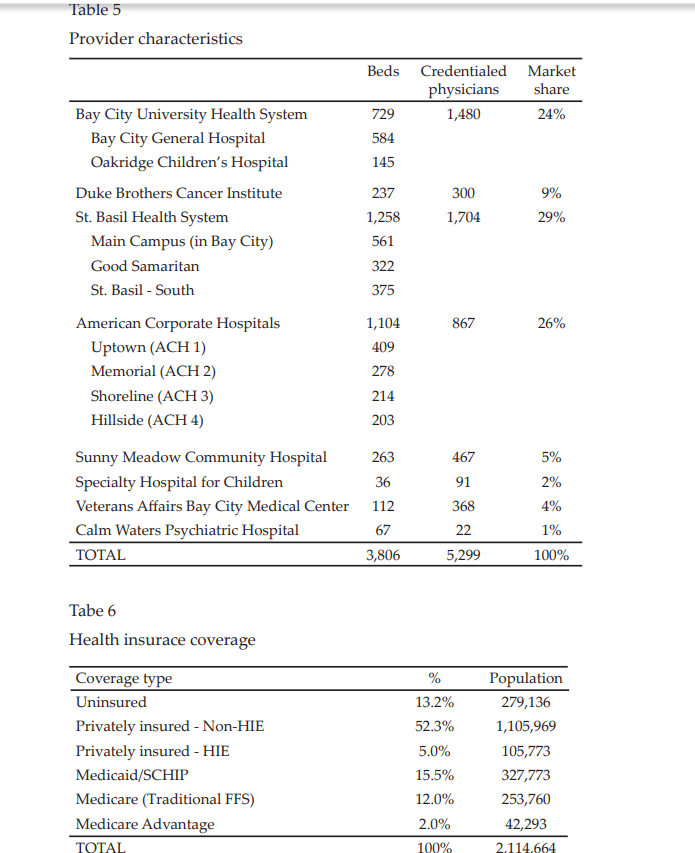
BCUHS operates two inpatient facilities on the same medical center campus: Bay City General Hospital and Oakridge Children's Hospital. Together, these account for 24% of the inpatient market in Apollo regional area, behind St. Basil Health System (29%) and American Corporate Hospitals (26%). Exceeding the average of the Apollo Bay regional area, the occupancy rate for Bay City General was a very healthy 78% last year. Although patients who are admitted to Bay City General are increasingly of higher acuity, inpatient volume has declined from where they were five years ago. Adjacent to Bay City General Hospital, Oakridge Children's occupancy rate was 67% last year, near the regional average. Admissions at Oakridge Children's have risen slightly (5%) over the last five years. Despite high-cost structure of running an AMC, the inpatient segment has been consistently, if only moderately, profitable for BCUHS. However, inpatient still returns for the largest total dollar profits for BCUHS. In the outpatient segment, BCUHS operates three ambulatory surgery centers, two specialty clinics, and more than 100 ambulatory clinics. While still smaller than inpatient in revenue and profit, the outpatient segment has consistently grown for BCUHS over the last 10 years. BCUHS has invested in heavily in establishing strong patient volume in outpatient services. The market for outpatient services, however, is highly fragmented. Competitors include organizations such as Bay City Clinic and dozens of smaller physician practice groups. The three fully accredited ambulatory surgery centers (ASC) are dispersed throughout Apollo Bay. One ACS is an endoscopy center, a joint venture between a gastroenterology and anesthesiologist physician group and BCUHS, that provides surgeries and colorectal cancer screenings for the community. The other two state-of-the-art medical technology ASC offer elective outpatient surgical procedures, such as hernia repair, arthroscopic joint repair, and cataract laser surgery. The specialty clinics include a 10-story Pediatric Clinical Sciences Building constructed seven years ago, a center for pediatric research and clinical care, and the Bay City Stroke Center, discussed below. BCUHS does not currently operate urgent care centers. BCUHS has not integrated Post-Acute Care (PAC) as a core component of their delivery system. While BCUHS operates Inpatient Rehabilitation Facilities (IRFs), this is generally only used following an acute episode of care. With the aging population, PAC services have been the fastest-growing health services segment in Apollo Bay. However, BCUHS does not own and operate skilled nursing facilities (SNFs). Rather, it contracts with several companies in the Apollo Bay regional area, most predominately EstateCare. Reimbursements are low in the PAC segment, and stability of EstateCare has recently been in question. Still, the care transitions from inpatient care to SNFs for individuals with disabling conditions is both ineffective and inefficient at BCUHS and in need of revamping.
Research translation
Research is a major component of the BCUHS mission. Not only does BCUHS use research innovation as a way to develop their brand, but they translate the research into new treatments and cures. To fund the research, BCUHS obtains grant funding from government organizations, such as the National Institute for Health and Agency for Healthcare Research and Quality; from foundations such as Josiah Macy Jr. Foundation and the Robert Wood Johnson Foundation; and from private industry, such as Bay City's Healthonics. Like many AMCs, BCUHS tries to balance government and foundation-funded research with industry-sponsored studies. In the recent past, BCUHS has explored a partnership with Healthonics to support their research mandate. Several patents have been filed, but so far no medical technology products have been brought to market. In addition, grant-funded innovations in health services management have successfully improved outcomes and reduced the costs of treatment. For example, one costly element of medical care in AMCs is the inclination to order too many diagnostic tests without concern for cost. Research into how to train medical residents to avoid this practice was piloted through a grant from a private foundation. After great initial success, these best practices were shared throughout the BCUHS operation with varying success. Furthermore, following the passage of the ACA, the BCUHS Department of Neurology practicing at the Bay City Stroke Center secured a three-year, $4 million grant from CMS's Patient-Centered Outcomes Research Institute to study the treatment options for reducing adverse effects of stroke among in African American and Hispanic patients. This comparative effectiveness research study hopes to improve treatment of stroke (O'Brien et al., 2015). Finally, at Oakridge Children's Hospital, a grant-funded partnership with the Bay County Health Department's Neighborhood Community Health Centers, developed a Center of Excellence for chronic disease management to increase access to primary care management for diseases like asthma and diabetes. The Center of Excellence included a mobile clinic, education fairs, and school-based programs.
Service lines
The highest volume service lines for Bay City General Hospital are women's care, cardiovascular, oncology (in partnership with Duke Brother's Cancer Institute), and neurology/stroke care. The women's care service line includes OB/GYN, maternal & fetal medicine, fertility services, and more. While it is a dependably profitable service line for BCUHS, American Corporate Hospitals has the largest market share due to aggressive marketing to expectant mothers in the Apollo Bay regional area. In the cardiovascular service space, St. Basil Health System dominates the market, but Bay City General is profitable despite the high costs of medical staff and technology. The BCUHS service lines that have minimal growth and inconsistent profits include orthopedics (high cost), endocrinology and diabetes (moderate cost), and rheumatology (low cost). Oakridge Children's Hospital is one of two pediatric-centered inpatient facility in the Apollo Bay area. (The other is the 36 bed Specialty Hospital for Children.) Oakridge Children's is the top-ranking facility in Bay City for pediatric congenital heart disorders, pediatric diabetes/endocrinology, neonatology, gastroenterology, and gastroenterology surgery. BCUHS's Bay City Stroke Center was established 15 years ago and earned Comprehensive Stroke Center designation 10 years ago from the American Heart Association/American Stroke Association and The Joint Commission. The collocated interprofessional team of doctors, including neurosurgery and vascular neurology, nurses, therapists, social workers, dietitians, and other specialized staff members provide emergency response services, surgical A population health strategy for Bay City 153 services, intensive care, and outpatient follow-up for stroke patients. BCUHS controls the largest share of the market for stroke-related services. In addition to strong profits and expected growth, the Stroke Center bolsters other neurology services, such as Alzheimer's disease treatment. Finally, Bay City General Hospital is the only Trauma 1 center in the state. A Level 1 Trauma Center is the highest level of certification by the Committee on Trauma of the American College of Surgeons. The certification requires 24- hour in-house coverage of a variety of physician specialties. Bay City General Hospital incurs great cost to maintain this service to the Apollo Bay regional area. BCUHS performs adult heart, lung, liver, kidney, and pancreas transplants, as well as pediatric kidney transplants. Legislation to expand trauma care to other hospital EDs has been unsuccessful over the last two years. St. Basil Health System and American Corporate Hospitals support the legislation; BCUHS opposes it.
Partnership with Bay County Health Department
Bay County Health Department (BCHD) is the lead public health agency in a regional cooperation between Bay, Taylor, and Lamar county health departments. The direct healthcare services provided by BCHD are delivered through the separately-branded (but BCHD-owned) Neighborhood Community Health Centers. This partnership allows BCHUS to bring high-quality medical practices to a low-cost setting while focusing on obtaining the best possible outcomes even while driving down costs. As a part of a contractual agreement, BCUHS places physician residents, medical students, dental residents, and nursing students in the three Neighborhood Health Centers in low-income neighborhoods of Apollo Bay regional area. The federally-qualified health centers (FQHCs) provide care to mostly primary care and chronic care services to uninsured and Medicaid-insured patients (Rothkopf, Brookler, Wadhwa, & Sajovetz, 2011).
Partnership with Duke Brothers Cancer Institute
BCUHS entered into a 10-year affiliation with Duke Brothers Cancer Institute 8 years ago. This affiliation agreement allows for BCUHS Department of Oncology faculty practitioners and researchers to be located primarily at the institute. The president of Duke Brothers Cancer Institute, Louis Winthorpe, III, M.D. holds a board director position at BCUHS. The agreement between organizations sets up areas of collaboration and clarifies financial exchanges. The Duke Brothers Cancer Institute research facilities are made available to all BCUHS faculty within National Cancer Institute guidelines and payment of fair-market lease costs. BCUHS manages all of the outpatient medical oncology infusion clinics for Duke Brothers Cancer Institute. While the relationship allows BCUHS to control the market for cancer care, the partnership dilutes the revenues and profits.
Clinical support services
The Bay City General Hospital emergency department (ED) has the largest volume of patients in the Apollo Bay regional area. Also, there is evidence that the Bay City General Hospital ED suffers from "adverse selection," meaning that they attract sicker and more resource-intensive patients, even controlling for diagnosis or procedure. Internal analysis shows that other EDs, especially those run by American Corporate Hospitals, are more likely to transfer patients without health insurance to the Bay City General Hospital ED after they've been stabilized, consistent with the EMTALA law (Rosenbaum, 2013). Despite the adverse selection problems, the ED generates important inpatient revenue for BCUHS. BCUHS currently has 55 operating rooms (40 in Bay City General and 15 at Oakridge Children's). At Bay City General, three operating rooms are state-of-the-art hybrid surgical suites that allow surgical teams to perform open and minimally invasive procedures in a single room. Two are combined cardiac surgery and catheterization labs, and the other combines MRI and surgical capabilities. While these investments in operating room technologies have been substantial, the surgery service lines continue to generate a large proportion of profits for BCUHS.
Technical and logistical support services
Over the last five years, BCUHS sought to maintain their position as a market leader through an increased emphasis on information technology. Millions of dollars have been invested in the implementation of an electronic health record (EHR) system that connected the inpatient facilities to its office-based physicians in the community. The EHR features include patient scheduling, computerized physician ordering entry, a population health reporting system, and more. Having completed the installation of its EHR system five years ago, many BCUHS physicians still complain about the additional time burden placed on them. However, an internal study found that the outpatient visits at BCUMG actually increased by almost 9%. BCUHS have enjoyed and promoted their top performance rankings over the years. However, now that the EHR allows detailed quantitative measures on outcomes that properly account for differences in case mix and other factors, BCUHS has realized that their performance may not be as exceptional as A population health strategy for Bay City 155 advertised. Given that the U.S. is entering an era in which performance data are directly tied to reimbursement, BCUHS will need to focus on improving outcomes rather than just relying on past reputation. BCUHS utilizes their Group Purchasing Organization (GPO) negotiated pricing agreements to various degrees, depending on the department and items purchased. For example, pharmacy uses GPO contracts over 80% of the time, but orthopedic purchases through GPOs only 35% of the time. Over the last three years, costs for supplies have increased 9.8%, more than any other cost category for BCUHS. Despite available opportunities for improved efficiencies, many physicians want to maintain relationships with medical supply vendors (e.g., medical device technologies). Some of the BCUHS providers notoriously want to use the latest and greatest medical devices without regard for quality outcomes or cost efficiency. Human resources, training, and development are centrally located at the BCUHS corporate offices on the main campus, which has enabled significant savings in administrative costs. As with many large organizations, managing the people resources is integral to performance. Despite challenges, BCUHS as shown success in addressing staffing needs. For example, there continues to be a shortage of experienced RNs in the Apollo Bay regional area. Yet, BCUHS improved its nursing vacancy rate from 22% three years ago to 12% this year. This was accomplished through a nurse retention initiative lead by the Chief Nursing Officer. This program included some wage increases for longer tenured employees, more flexible schedules, and a leadership development programs. This success was achieved despite the previous BCUHS CEO declining to apply for the American Nurses Credentialing Center Magnet Recognition Program.
Bay City University Medical Group (BCUMG)
The Bay City University Medical Group (BCUMG) functions as a unified, integrated faculty practice within BCUHS. BCUMG provides clinical operations through which 1,400-plus physicians provide medical care to patients at the two hospitals, three ambulatory surgery centers, two specialty clinics, and over 100 ambulatory clinics. Approximately 30% of the physicians of BCUMG are primary care providers and 70% are specialists.
Ancillary services at BCUHS
Like the other health systems, laboratory services are operated internally at BCUHS. Over the last three years, lab services have outpaced all others' growth within the health system. The reason for this growth is the implementation of a laboratory information system (LIS) which enables connections between the BCUHS LIS and EHR systems of its office-based physicians. Fortunately, the new EHR, combined with clinical informatics, has allowed BCUHS to significantly reduce unnecessary lab testing. This has increased profitability associated with risk payment contracts. Also, BCUHS has actively promoted lab services to other non-BCUHS community physicians, and has successfully gained market share from other competing lab services, such as Mission Diagnostics, Inc., American Laboratories, and St. Basil Health Lab Services. Similarly, health information technology enhancements in medical imaging at BCUHS has improved efficiency and profitability. Last year brought a newly implemented integrated Picture Archiving and Communications System (PACS) and a Radiology Information System (RIS). This significant investment enables BCUMG outpatient sites to register patients, schedule appointments, order test, and access and archive imaging tests with improved workflow efficiency. This system has been touted as the model for improved medical care coordination within the health system.
Bay City market overview
Health systems
Considered highly consolidated, most of the 14 impatient facilities in the Apollo Bay regional area are linked in some way to the three large delivery systems. Competition among these health systems is strong, but generally cooperative. Hospitals no longer act as independent inpatient facilities, but, rather, integrated regional networks focused on delivering care across the continuum of care. However, since most physicians have privileges at more than one hospital in the region, and hospitals all provide similar services, there is no sense of advantage.
Inpatient care
The 14 inpatient facilities are staffed with 3,806 beds total (1.8 hospital beds per 1,000 population). Last year, the average length of stay (ALOS) was 5.7 days with an average occupancy rate of 70.9%. Three major delivery systems - BCUHS, St. Basil Health System, and American Corporate Hospitals - provide the vast majority of care in the regional area, at 24%, 29%, and 26% market share, respectively. BCUHS includes a main campus hospital, Bay City General Hospital (584 beds), and children's hospital, Oakridge Children's Hospital (145 beds). The non-profit St. Basil Health System includes three hospitals, St. Basil Hospital (561 beds), Good Samaritan Hospital (322 beds), and St. Basil Hospital - South (375 beds). The area's other non-profit hospitals are Sunny Meadow Community Hospital (263 beds), Specialty Hospital for Children (36 beds), and Duke Brothers Cancer Institute (237 beds). There are two government-run facilities, the federal Veterans Affairs Bay City Medical Center (112 beds) and the staterun Calm Waters Psychiatric Hospital (36 beds). The for-profit hospital chain, American Corporate Hospitals, has four inpatient facilities in the Apollo Bay regional area, Uptown (409 beds), Memorial (278 beds), Shoreline (214 beds), and Hillside (203 beds). Hospitals in the region are paid in a variety of manners. Medicare pays hospitals based on diagnosis related groups (DRG) adjusted upward if there are existing comorbidities. These prospective payments incentivize the hospitals to minimize the costs associated with the patient stay. With the passage of ACA, Medicare implemented pay-for-performance programs that pay hospitals based on controlling costs and meeting quality targets. No hospitals in Bay City have created a Medicare ACOs for the Shared Savings pay-for performance program funded by the Affordable Care Act. Private insurance companies, however, pay hospitals fee-for service. For each service, the insurers pay a discounted rate based on the charges that the hospital submits on their electronic claim. Similarly, payment for Medicaid patients, financed exclusively by managed care plans, are negotiated separately with each company. Depending on the sophistication of the health plan, the payment is either based on Medicare DRGs, but deeply discounted, or paid per diem (set amount per night).
Emergency care
All of the aforementioned hospitals run emergency departments (EDs) in the Apollo Bay regional area. These EDs have higher utilization rates than other EDs across the state. Similarly, the EDs in Bay City are utilized more often for less severe cases than other EDs in the state.
Physicians
There are 4,377 physicians practicing in the Apollo Bay regional area including both allopathic physicians (MDs) and osteopathic physicians (DOs). There are 1,734 primary care physicians and 2,643 specialist physicians. Many physicians hold privileges at more than one inpatient facility and/or health system. However, the supply of well-trained health physicians is increasingly inadequate. There are fewer physicians in Apollo Bay regional area for its population size than the national rate, including fewer primary-care physicians. Solo and small-group practices are giving way to larger groups as physicians sell their practices or affiliate with provider networks. There are still a collection of smaller private specialist groups that exist in the Bay City area. These conservative independent physicians favor "pure competition" and the financial benefits they currently derive from the three hospital systems bidding against each other. Regional area providers contracting with health plans in the commercial insurance market are typically paid on a fee-for-service basis. Specifically, physicians submit claims to insurers electronically with Current Procedural Terminology (CPT) codes that indicate the type of service provided in the outpatient visit and the International Classification of Diseases codes (ICD) that indicates the patient diagnoses. The small set of CPT codes that primary care providers typically bill for are usually called "evaluation and management (E&M)" codes. The fee-for-service payment approach encourages increased volume of care (Schroeder, Frist, & Natl Commission Phys Payment, 2013). Medicare also pays providers based on fee-for-service CPT codes. However, Medicare uses a fee multiplier to adjust for physician work, practice expense, and malpractice expense. These so-called relative value units tend to overvalue procedures associated with specialists at the expense of patient care coordination associated with primary care (Ginsburg, 2012). Fee-for-service is not universal in Bay City, however. Some physician groups, such as Bay City Clinic, have made capitation-based contract arrangements with private and Medicare Advantage insurers. Capitation incentivizes the physician groups to reduce costs of care they deliver. Solo or small physician groups with smaller numbers of patients are less likely enter into capitation contracts, as the ability to spread risk is diminished.
Registered nurses
Persistent nurse shortages in the area are a major operational concern for the health system in Bay City. However, some early-career registered nurses (RNs) report problems finding jobs. Even so, wages for experienced RNs have consistently risen throughout the region. The area healthcare leaders have expressed concern that, just as the baby boomers age and begin to consume more healthcare, the older nurses will begin to retire (Auerbach, Buerhaus, & Staiger, 2015). The BCUHS School of Nursing, one of the most selective in the state, graduates almost 400 bachelors-prepared RNs each year. Another 400 bachelors-prepared RNs graduate from several other colleges in the area. Area community colleges also graduate roughly 200 associate-level RN programs. Less than 15% of the new hires at Apollo Bay regional area inpatient hospitals are associate-level RNs.
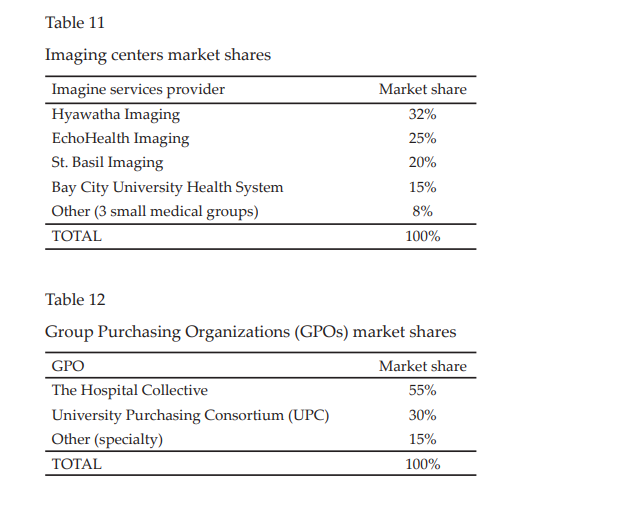
Diagnostic imaging
Diagnostic imaging services include advanced magnetic resonance imaging (MRI), computed tomography (CT) scan, positron emission tomography (PET) scan, nuclear medicine, ultrasound testing, X-ray, echocardiogram (ECHO), and electrocardiogram (EKG). The diagnostic imaging revenue will probably only grow slightly due to continued reimbursement cuts and more conservative treatment decisions by physicians, even with increasing volume expected from aging population. Hyawatha Body Imaging is the largest imaging company in the region with a full portfolio of technologies offered at their 10 locations. EchoHealth Imaging, known as the low-cost, high-volume vendor, is the second largest provider of diagnostic imaging. Two large health systems, St. Basil Health System Imaging and BCUHS, also provide imaging services. BCUHS is known to have the cutting-edge technology for diagnostic imaging.
Pathology and laboratory
The pathology and laboratory market segment includes phlebotomists drawing blood at outpatient locations to pathologists and medical technologists/technicians testing samples in centralized or regionalized laboratories. The national for-profit companies, Mission Diagnostics, Inc. and American Laboratories, hold over half the market share, and the health system-based operations of St. Basil Health Lab Services and BCUHS share another a third of the market. The smaller independent physician-owned Rushing Falls Pathology Services Corporation has an exclusive contract with Sunny Meadow Community Hospital.
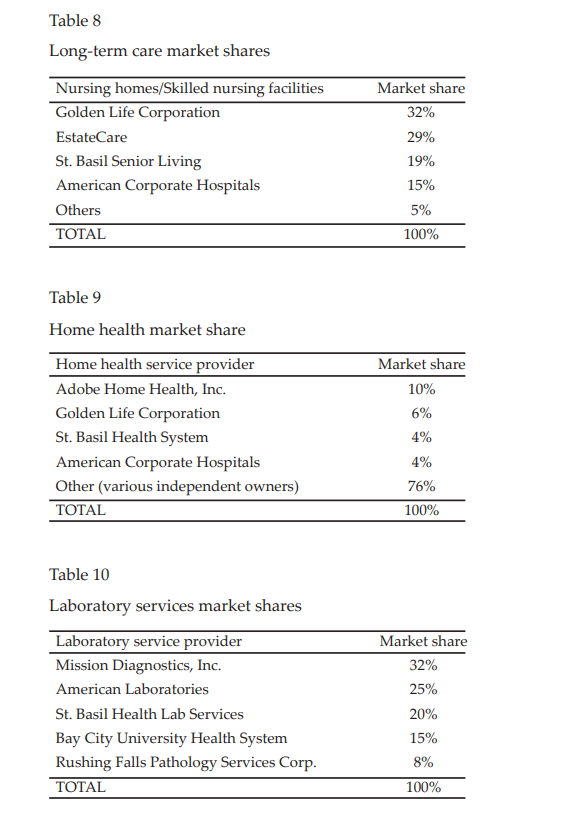
Post-acute Care (PAC)
Post-acute Care (PAC) is provided in various settings, including home-health, nursing facilities, inpatient rehabilitation facilities, and long-term acute care hospitals. There are over 60 nursing facilities in Apollo Bay regional area with approximately 5,000 beds. There have been very low occupancy rates (
Purchasing groups
Group Purchasing Organizations (GPOs) aggregate hospital and healthcare provider purchasing power and use that leverage to negotiate discounts with manufacturers for supplies such as pharmaceuticals, bandages, biologics, etc. In the Apollo Bay regional area, two GPOs account for 85% of the hospital market: The Hospital Collective (55%) and University Purchasing Consortium (30%). Both claim to offer the best product for the best price, superior leverage with suppliers, and the ability to analyze pricing throughout the supply chain. These GPOs emphasize "total supply chain management," the overall process by which products are ordered, delivered, inventoried, purchased, used, and disposed.
BCUHS Affiliates and Competitors
Bay County Health Department
Bay County Health Department (BCHD) is the lead public health agency in a regional cooperation between the Bay, Taylor, and Lamar county health departments. BCHD provides typical health department functions, such as regulation, inspection, licensing, food safety education, and maternal and child health services. BCHD provides population-based primary prevention services, such as nutrition and tobacco cessation programs. Also, screening for diseases or conditions, such as tuberculosis and high blood pressure, is a common service offered by BCHD. Finally, BCUHS provides maternal and child health services, such as WIC, maternal and child home visits, family planning, and Early and Periodic Screening, Diagnostic and Treatment (EPSDT), which is Medicaid's child health component. The direct healthcare services provided by the health department are delivered through the separately-branded (but BCHD-owned) Neighborhood Community Health Centers. These clinics operate in low-income areas of the region. The clinics are federally qualified health centers (FQHC), meaning that they are financially subsidized by the government to act as safety-net providers for vulnerable populations. Medicaid pays the largest share of the total revenues to Neighborhood Community Health Centers. BCHD has operated at a financial loss for three out of the last five years. While low reimbursements by Medicaid and the high proportion of bad debt contribute to the financial burden, the losses are partly due to poor operational effectiveness by BCHD management. As a part of a contractual agreement, BCUHS places physician residents, medical students, dental residents, and nursing students in three Neighborhood Health Centers in the area.
Duke Brothers Cancer Institute
Duke Brothers Cancer Institute (DBCI) opened in 1992 with a $200 million posthumous donation from the Duke & Duke commodity trading company founders, Randolph and Mortimer Duke. While the DBCI was opened with auspicious plans to eventually qualify as a National Cancer Institute Comprehensive Care Center, a series of financial setbacks has delayed their plans. Nonetheless, the dynamic Dr. Louis Winthorpe, III, President of Duke Brothers Cancer Institute, has made moves to improve the market position of DBCI by affiliating with the preeminent BCUHS. In exchange for sharing research resources and technologies, DBCI received ability to apply to the federal government for more significant research grants. This partnership has worked very well despite the decrease in federal research funding available in recent years. Dr. Winthorpe has been a director of BCUHS Board of Directors for five years.
St. Basil Health System
BCUHS' competitor, St. Basil Health System, is named for the patron saint of hospital administrators, St. Basil the Great. In order to compete in a highly regulated industry as healthcare, St. Basil Hospital merged with Good Samaritan Hospital in the mid-1990s, forming St. Basil Health System (SBHS). In 2001, SBHS built St. Basil - South in a suburban Bay City location. Now, SBHS has the largest inpatient market share in Apollo Bay regional area with 29%. St. Basil Health System renovated many of its existing, aging facilities in recent years. The health system is also considering replacement plans for the primary hospital space in downtown Bay City with a suburban location within the next 10 years. SBHS touts itself as an integrated delivery system. SBHS owns St. Basil Health Plans covering over 77,000 commercial lives. Also, SBHS owns and operates St. Basil Home Health Care, St. Basil Senior Living nursing homes, and St. Basil CarePartners, the medical practice group. St. Basil CarePartners has more than 125 locations in the region, including a new medical building that aims to integrate primary care with specialist care. SBHS is known for its Heart Center, a service line that dominates the Apollo Bay regional area market. They had the incumbency advantage in interventional cardiology for a decade, and have an advantage with brand identity when it comes to heart surgery. SBHS owns and operates an imaging services company called St. Basil Imaging. SBHS stated that their facilities had expanded to handle additional capacity throughout the Bay City area, so they decided to consolidate imaging services in Apollo Bay regional area at their own facilities. The health system terminated its contracts with other imaging companies in the area, Bay Citybased EchoHealth Imaging and Hyawatha Body Imaging. This move was said to ensure that the diagnostic imaging business would be conducted within its own facilities. SBHS also owns and operates their own laboratories, but maintains contracts with other vendors, such as Mission Diagnostics, Inc. and American Laboratories.
American Corporate Hospitals
American Corporate Hospitals (ACH) is one of the largest investor-owned for-profit hospital companies in the world, and it operates five inpatient facilities in Apollo Bay regional area. The administrative offices for ACH are in downtown Bay City with hospitals throughout the region, particularly in higher-income areas. Uptown Hospital (409 beds) also operates the second-largest emergency department (ED) in the region (Bay City General Hospital ED is the largest). A recent controversy was reported in the area newspaper that the Uptown ED was treating paying customers and leaving the self-pay and indigent patients to be treated by Bay City General Hospital. Statistical analysis by the state regulatory agency did not confirm these accusations. In addition to the 5 inpatient facilities operated by the for-profit chain in the regional, ACH also owns 17 urgent care centers, 5 outpatient surgical centers, and 12 retail clinics in partnership with a local retail pharmacy company. The urgent care centers are typically staffed by physicians with backgrounds in primary care or emergency medicine, and the retail clinics are staffed with nurse practitioners or physician assistants working under physician supervision. These facilities do not accept uninsured patients, unless self-paid, nor Medicaid insurance.
Sunny Meadow Community Hospital
Sunny Meadow Community Hospital (SMCH) has struggled to maintain its independence over the last decade. With declining revenues and market share, SMCH brought in a consulting firm to help them cut costs through a "performance improvement plan." However, some saw this as a way to cut nurse salaries and increase nurse-to-patient ratios. Within the past year, in exclusive collaboration with the health insurer VitaNation Health, SMCH acts as the "preferred" hospital for their health plan enrollees (other hospitals are available for higher copayments). This arrangement does not involve any innovation in payment methods for SMCH. It is almost entirely fee-for-service. In fact, SMCH has eliminated all capitation contracts with health insurance companies, due to the financial risk involved.
Bay City Clinic
Bay City Clinic is an independently owned multi-specialty physician corporation with more than 30 specialties, 200 providers, and 46 different office locations. Physicians maintain privileges at hospitals at St. Basil Health System and American Corporate Hospitals.
Bay City health insurance market
Health insurers also compete in several different market segments in the Apollo Bay regional area, including the private (commercial), the Health Insurance Exchange (ACA marketplace), Medicaid managed care, and Medicare Advantage markets. Most people in Bay City are covered by commercial health insurance either through their work (52.3%) or through the Health Insurance Exchange (5.0%). Medicare (12%) and Medicare Advantage (2.0%) cover those age 65 and over and some disabled individuals. Medicaid, for low-income individuals, and SCHIP, for low-income children not quite eligible for Medicaid, cover 15.5% of the population. Even after the implementation of the ACA, 13.2% of the population is uninsured.
Commercial health insurance
The four leading commercial plans are InsuraCare Health, VitaNation Health, Health Matters Health Plans, and St. Basil Health Plans. In addition to the four leading plans, the commercial market has an abundance of smaller companies. While these health plans try to differentiate themselves from one another, all use overlapping medical provider networks. Commercial health plans target businesses that offer health insurance to their employees. These businesses pay insurers a set amount per employee based on their predicted health service use, called underwriting. Some commercial plans sell health insurance to individual, but this market is shrinking due to the introduction of the ACA's Health Insurance Exchange.
Medicaid managed care
Medicaid, the health insurance for low-income people, and SCHIP, the health insurance for children who don't qualify for Medicaid, is financed by both federal and state funds. The state contracts with private managed care plans to organize and finance the care for those individuals insured by Medicaid and SCHIP. Provider networks of the Medicaid managed care organizations overlap significantly - about one third of hospitals and one half of primary care physicians contract with multiple Medicaid managed care organizations. Comprehensive Health Plan serves approximately 100,000 members in the regional area. Comprehensive Health Plan executives have been in the news lately regarding violations of financial regulations required by the state. Specifically, the health plan did not meet the capital reserve requirements, so they temporarily had their enrollment of new members frozen. Also, healthcare providers have been complaining that Comprehensive Health Plan has been slow to pay claims, although the state regulatory denied that they were out of compliance. An expos in the Bay City Courier revealed that the health plan had been holding high-dollar claims in order to review them, but reviews were taking longer than 60 days, according to Bay County Health Department's Neighborhood Community Health Clinics operations manager.
Medicare Advantage
Medicare Advantage enrollment represents approximately 20% of the total Medicare beneficiaries in the area, and the rest are served by traditional Medicare (fee-for-service). Capitation contracts among outpatient physicians and some hospital networks continue to be a feature of the Medicare Advantage market.
Affordable Care Act's state health insurance exchange
The state health insurance exchange, CoverState, was created under the Affordable Care Act. The state-built online marketplace was plagued by technical difficulties, so the legislature voted last year to switch to the federally-built HealthCare.gov. The health insurance companies that participated last year chose to continue in the health insurance exchange this year. The average premiums charged by these insurers declined 2.5%. The state limits the number of health insurers that can participate in the exchange, although the state regulating committee indicated that more than four health insurance companies would be allowed to participate in the next application period. Participating health insurers are required to offer bronze, silver, and gold benefit-level plans. Platinum plan offerings are optional. All geographic areas of the state must be represented. Individuals can shop for insurance on the Health Insurance Exchange website.
Apollo Bay regional area characteristics
Population Characteristics
Bay City is a vibrant community known for its friendly people and beautiful setting by Apollo Bay. With a growing population of more than 600,000, Bay City offers many public spaces for exercise and entertainment, interesting early 20th century architecture, and one of the best universities in the state. The Apollo Bay regional area spans three counties (Bay, Lamar, and Taylor) with a total population of over 2 million. The employer community is characterized by mostly small- and mediumsized businesses. The largest employers are in the public sector: federal and state governments, public schools, and a State University. The largest private employer in the regional area, Healthonics, has its operational headquarters in suburban Bay City. Healthonics is the world's fourth-largest medical device company with more than 50,000 employees, including some 6,000 based in Bay City. Small population growth is expected for individuals aged 18 to 44 (3.2%), moderate population growth for individuals aged 0 to 17 (5.8%), and strong growth for those 45 to 64 (9.2%). Population growth for individuals aged 65 and older is expected to grow substantially (21.2%). See the table "Age Distribution of Apollo Bay regional area." Last year, the official poverty rate for the region was 14.5%, slightly above the national average. The most common race/ethnicity in the regional area is white (51.8%), followed by Hispanic (26.5%), African American (15.6%), Asian (3.7%), individuals of two races (1.9%), and other (0.5%). Substantial growth is expected for the Asian (20.6%), Hispanic (17.5%), individuals of two races (15.0%), and African American (10.7%) populations, while marginal growth is expected for the white population (0.5%).
Community health characteristics
Apollo Bay regional area has a higher prevalence of both adults and youth diagnosed with asthma than other areas of the state and the United States as a whole. The prevalence of adults in Apollo Bay regional area diagnosed with diabetes is slightly less than for adults in the state. However, diabetes is higher for adults in Apollo Bay regional area than for adults in the U.S. as a whole. There is also a higher prevalence of obesity among Apollo Bay regional area adults. Among the Hispanic and African American residents in Bay City, children have higher rates of obesity than the white population, and the prevalence has increased over the last three decades. In the African American community, over 39% of children are overweight or obese, and 37% Hispanic children, compared to 30% of white children. Among children aged 9-13 years, 24.1% of blacks and 25.9% of Hispanics are involved in organized physical activity outside of school compared with 46.6% of whites. Heart disease is the leading cause of death in Apollo Bay regional area, with a mortality rate higher than the rest of the state. The region's heart disease death rate is higher than the Healthy People 2020 Goal and ranks between the 25th and 50th percentiles. The percentage of adults in Apollo Bay regional area who reported high cholesterol is nearly three times the Healthy People 2020 Goal and ranks between the 25th and 50th percentiles. The percentage of Apollo Bay regional area adults who reported smoking is substantially higher than the Healthy People 2020 Goal. Cancer is the second-leading cause of death in Apollo Bay regional area. The top five cancer mortality rates are lung, colon, breast, pancreatic, and prostate. The percentages of adults receiving tests for cervical, breast and colorectal cancers higher than state and national percentages. However, screening for prostate cancer was lower than state and national percentages. There is a similar disparity in Bay City for asthma among African American children who have twice the rate of emergency department visits and hospitalizations for asthma as white children. Also, percentage of children with asthma taking to asthma control medications is lower among Hispanics (23.2%) and African Americans (25.1%) than among Whites (35.1%). Infant mortality rate, preterm birth rate, and infant birth weights are all important measures of the care pregnant women and their newborns receive during pregnancy. In 2009, the March of Dimes gave Apollo Bay regional area an "F" for its efforts to reduce preterm births. The state is ranked 32nd among the 50 states, Puerto Rico, and the District of Columbia.
Policy developments
Patient Protection and Affordable Care Act (ACA)
The Patient Protection and Affordable Care Act of 2010 may be the most significant piece of legislation since the Social Security amendments created Medicare and Medicaid in 1965. The impacts on the healthcare industry will continue to be significant. In addition to helping to insure millions more people in the U.S. through the Health Insurance Marketplace and Medicaid expansion, the law experiments with encouraging value in how providers and insurers are paid, boosting research comparing the effectiveness of different treatments approaches, and promoting population-based activities.
Medicare Accountable Care Organizations (ACOs)
The Affordable Care Act created a new pay-for-performance initiative within Medicare called the Shared Savings Program. With this program, the Centers for Medicare and Medicaid Services (CMS) wants to move "increasingly toward rewarding better value, outcomes, and patient-centered care instead of merely volume." CMS intends for the Medicare Shared Savings Program to encourage integration among providers and hospitals. To participate in this Medicare program, new organizations, called Accountable Care Organizations (ACOs) must be created. If the ACO reduces costs relative to certain illness severity-adjusted expenditure benchmarks, then the savings are split between Medicare and the ACO. The bonus is only shared as long as the ACO meets the quality measurement thresholds. The organization must have a formal legal structure to receive and distribute the shared savings bonuses to individual providers. Also, they must have a sufficient number of primary care professionals for the number of assigned beneficiaries (5,000 at a minimum). Furthermore, ACOs must demonstrate clinical and administrative management structures to coordinate care for patients. PCPs may only participate in one ACO and hospital, but hospitals and specialist providers can participate in more than one. The ACO must report the necessary data to evaluate quality and cost measures. Finally, the ACO must demonstrate it meets patient-centeredness criteria, such as using electronic health records and communicating evidence-based medicine. The Apollo Bay regional area does not yet have an ACO operating in the Shared Savings Program.
Medicaid expansion
Under the ACA, states had the option to expand Medicaid coverage to 138% of the federal poverty level (FPL) for individuals under age 65. While the Supreme Court ruling made the ACA Medicaid expansion provision optional to the states, Bay City's state government elected to expand the Medicaid eligibility threshold (just over $33,000 for a family of four last year). The expansion covered roughly 240,000 newly eligible and 20,000 previously eligible residents, bringing the total to more than 327,000 low-income individuals. The expansion may have a less pronounced impact than in some states since the state already covered some childless adults with incomes up to 10% of FPL.
Medicaid Coordinated Care Organizations (CCOs)
The Affordable Care Act legislated pilots of new coordinated care organizations (CCOs) that combine Medicaid/SCHIP managed care plans and provider organizations to increase accountability for the health of the population. Modeled after Medicare Shared Savings Program's Accountable Care Organizations, CCOs are required to integrate and coordinate treatment. CCOs will be paid based on a per-member-per-month capitation rate. The capitation rate will cover all physical, mental, and dental care, as well as pharmaceuticals. However, the capitation rate will exclude long-term care services. This program is different from the current Medicaid/SCHIP managed care plan in that there is a single global payment, instead of a capitated rate for each different type of care (physical, mental, etc.). Also, the providers and insurers must be legally a part of the same organization, as opposed to entering into a contractual relationship, as in the managed care model. This means that CCOs are afforded the flexibility to provide care without the need to get services approved by managed care companies. The population covered by CCOs include Medicaid and SCHIP. Within the Medicaid recipients, both the Temporary Assistance for Needy Families (TANF) and Social Security Income (SSI) populations will be included. The rates for TANF, typically healthy mothers and their children, are much lower than for SSI, predominantly sicker and disabled patients. The state actuaries will use a risk-adjustment methodology to arrive at rates each group and geography. That is, the rates will be adjusted based depending on the health of the CCO patient population. Also, there is a pay-for-performance component that rewards CCOs for meeting quality targets, as determined by the state. The performance measures will incentivize preventive care and chronic care management. To become a CCO, an organization must submit an application to the state that demonstrates their information technology system, coordination of care capabilities, and the adequacy of their provider network.
Medicare readmission penalties
The Readmission Reduction Program was legislated in Section 3025 of the Affordable Care Act. Regulations for this law penalize hospitals where patients discharged and readmitted within 30 days with the same diagnosis for health conditions such as pneumonia, myocardial infarction, and heart failure. The penalty is a percentage deduction from their Medicare payments up to 3%. Some hospitals, particularly those that serve economically disadvantaged populations such as BCUHS, are concerned about the methodology for measuring readmissions. It is the CMS position that these hospitals should be able to make improvements in care delivery to reduce avoidable readmissions.
Health Insurance Exchanges
Probably the biggest policy change brought by the ACA is the creation of Health Insurance Exchanges (HIE). HIEs serve as portals through which individuals and small businesses can compare and purchase health insurance. There are standardized benefit levels designed to cover a certain amount of an individual's statistically predicted health expenses. The levels are termed "platinum," "gold," "silver," and "bronze." So far, four companies in Apollo Bay regional area are participating in the HIE, offering a variety of benefit plan levels. As a part of the ACA, individuals are required purchase a qualified health plan or face a penalty. If premiums are more than an individual can afford, the federal government will subsidize the cost, financing a portion of the individual's health insurance cost. Without the mandate, many healthy individuals would not enroll in insurance plans, and the plans would suffer from "adverse selection." If the majority of the new enrollees are unhealthy, the money insurers collect in premiums would not be enough to cover claims and premium rates would skyrocket. The most recent enrollment numbers for the state show that more than 105,000 people have enrolled in plans through the HIE. Despite subsidies for those that qualify and penalties for not getting covered, almost 280,000 people in the region remain uninsured. States could have established and run the exchange in their state, or they could have let federal government run it. CoverState, the state's health insurance exchange, decided to build and run their own HIE, but operational problems led the state to change course and use the federally-build system after one year.
Certificates of Need
The number inpatient beds available in Apollo Bay regional area is controlled by regulators in the state through a process called Certificate of Need (CON). The CON laws were first developed in the state in the 1970s with the goal of slowing medical spending. Currently, to expand the number of beds in the area, an independent market appraisal would have to determine that there is a need for an increased number of inpatient beds. Applications by qualified applicants would be reviewed by state regulators and independent review committees and awarded on merit.
Mandated nurse-to-patient ratios
In the last two legislative sessions, a bill in the state house was proposed that would mandate nurse-to-patient ratios at hospitals in the state. While the bill did not pass the State House and never came for a vote in the State Senate, the potential move had hospital executives in Bay City concerned. The State Nurses Association did not support the bill to mandate the patient-to-nurse ratios at certain levels depending on the type of inpatient unit. However, there has been an effort led by the AFL-CIO in the state to unionize nurses, and the AFL-CIO supports mandated nurse-to-patient ratio minimums.
Step by Step Solution
There are 3 Steps involved in it

Get step-by-step solutions from verified subject matter experts


