Question: Case Study and Exhibit #2 please please help me answer all the questions to double check my work! THANK YOU! Background In the ClearEyes Cataracts
Case Study and Exhibit #2
please please help me answer all the questions to double check my work! THANK YOU!
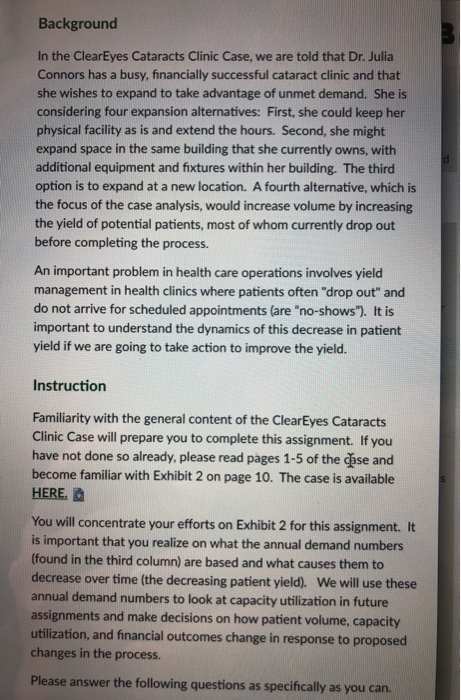
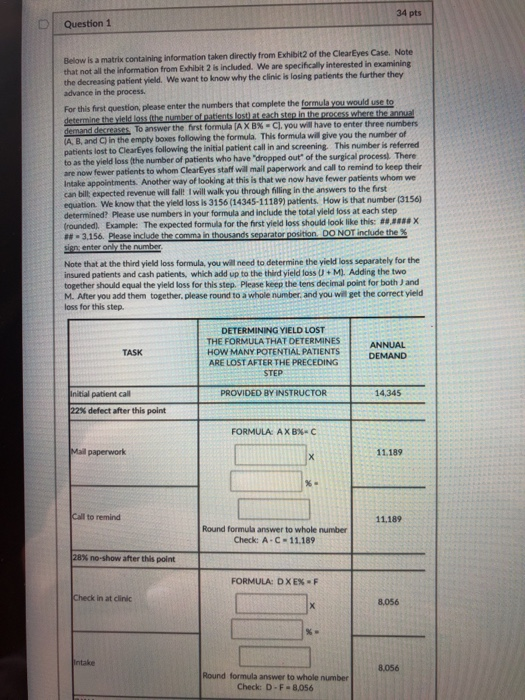
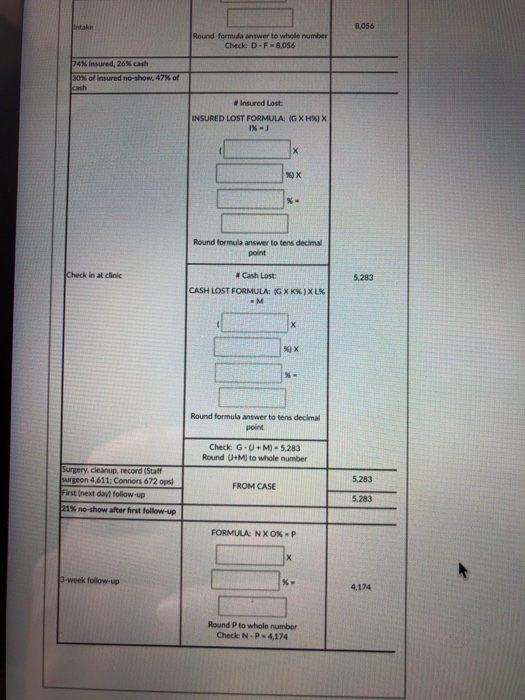
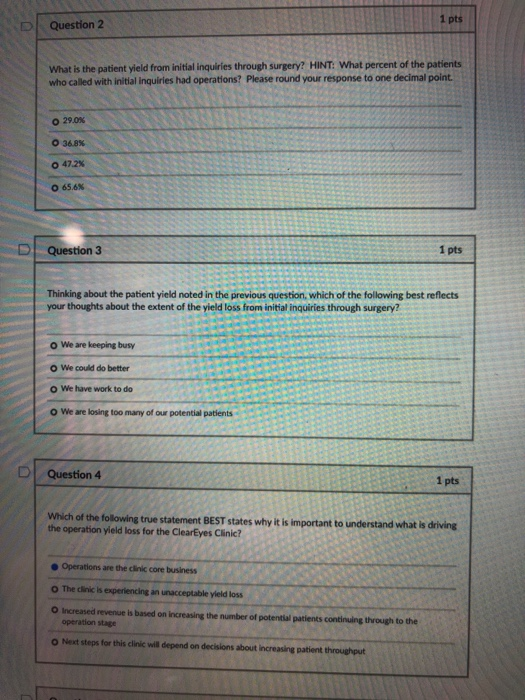
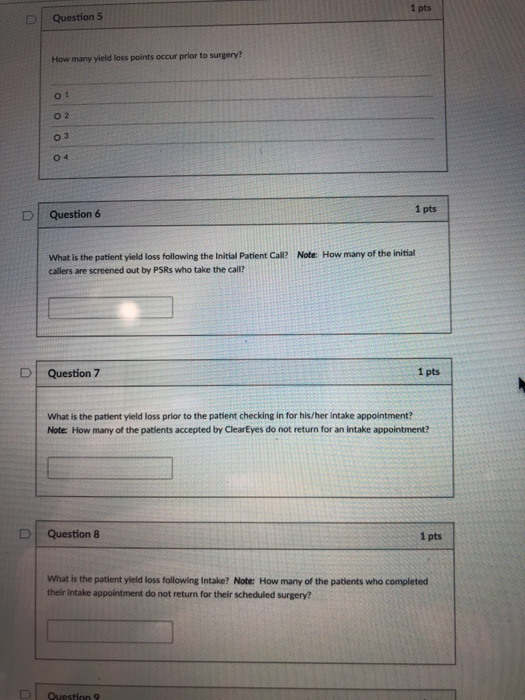
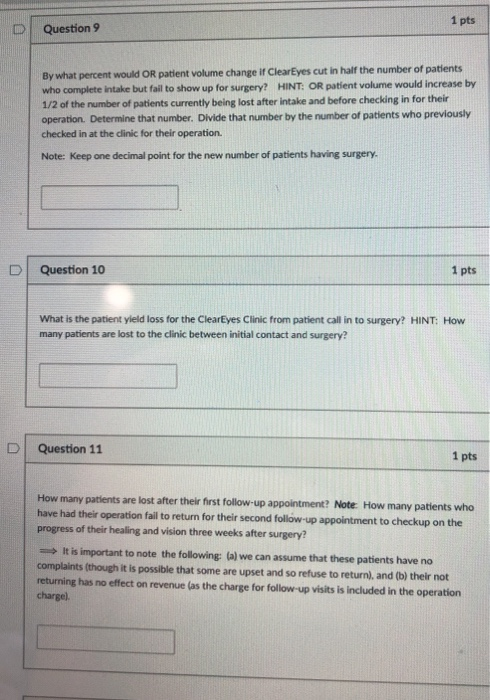
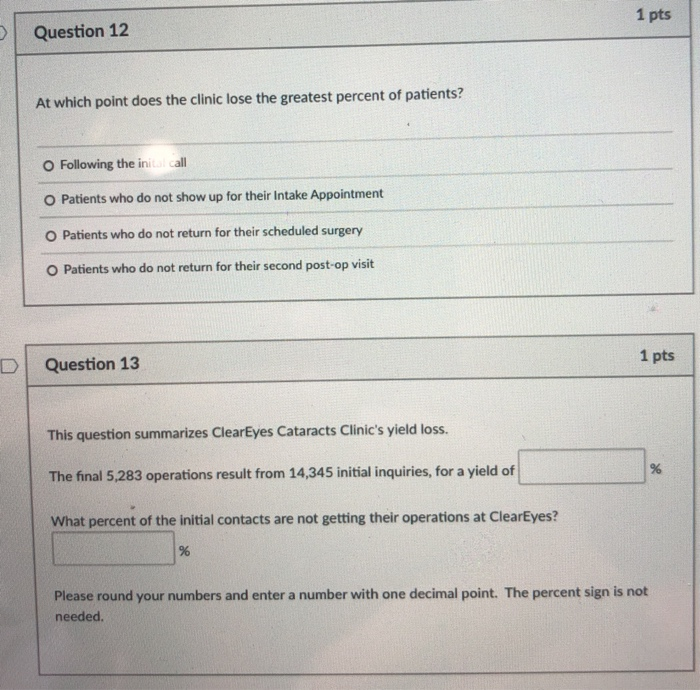
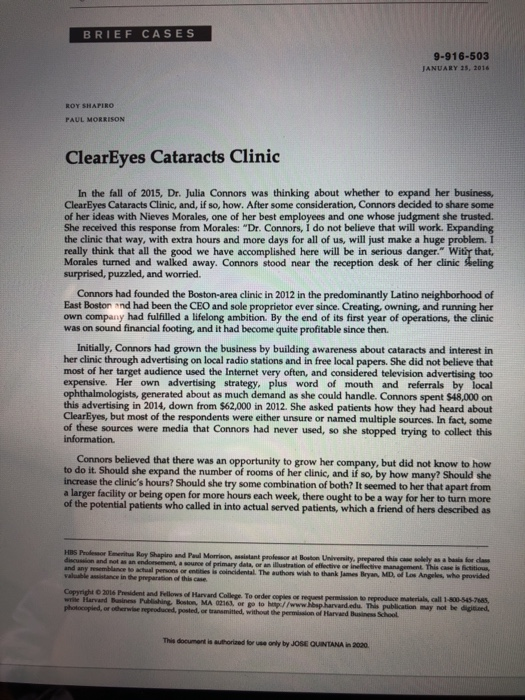
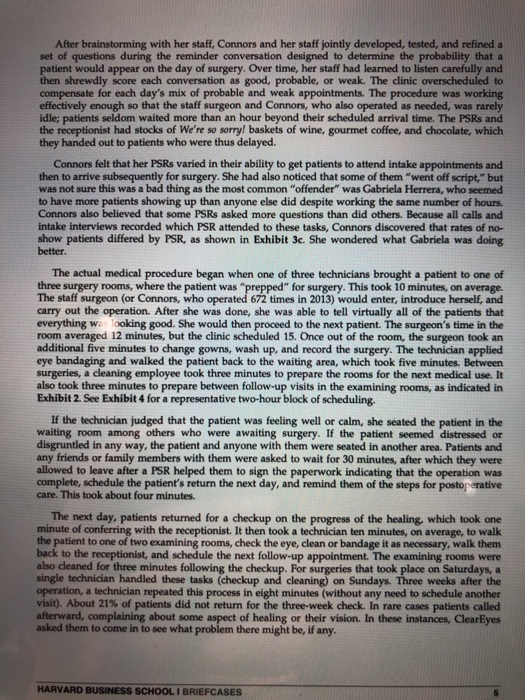
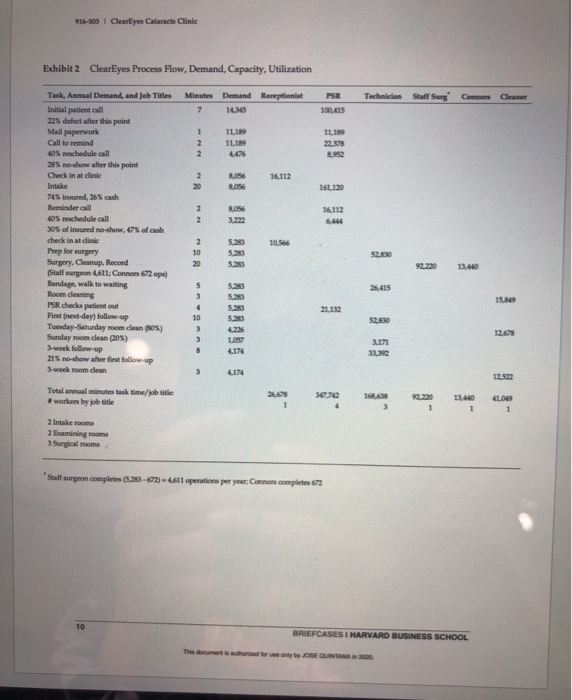
Background In the ClearEyes Cataracts Clinic Case, we are told that Dr. Julia Connors has a busy, financially successful cataract clinic and that she wishes to expand to take advantage of unmet demand. She is considering four expansion alternatives: First, she could keep her physical facility as is and extend the hours. Second, she might expand space in the same building that she currently owns, with additional equipment and fixtures within her building. The third option is to expand at a new location. A fourth alternative, which is the focus of the case analysis, would increase volume by increasing the yield of potential patients, most of whom currently drop out before completing the process. An important problem in health care operations involves yield management in health clinics where patients often "drop out" and do not arrive for scheduled appointments (are "no-shows"). It is important to understand the dynamics of this decrease in patient yield if we are going to take action to improve the yield. Instruction Familiarity with the general content of the ClearEyes Cataracts Clinic Case will prepare you to complete this assignment. If you have not done so already, please read pages 1-5 of the case and become familiar with Exhibit 2 on page 10. The case is available HERE. You will concentrate your efforts on Exhibit 2 for this assignment. It is important that you realize on what the annual demand numbers (found in the third column) are based and what causes them to decrease over time (the decreasing patient yield). We will use these annual demand numbers to look at capacity utilization in future assignments and make decisions on how patient volume, capacity utilization, and financial outcomes change in response to proposed changes in the process. Please answer the following questions as specifically as you can. 34 pts Question 1 Below is a matrix containing Information taken directly from Exhibit2 of the ClearEyes Case. Note that not all the information from Exhibit 2 is included. We are specifically interested in examining the decreasing patient yield. We want to know why the clinic is losing patients the further they advance in the process. For this first question, please enter the numbers that complete the formula you would use to determine the viel loss the number of patients lost at each step in the process where the annual demand decreases to answer the first formula (AXBX-Cl. you will have to enter three numbers A, B, and in the empty boxes following the formula. This formula will give you the number of patients lost to ClearEyes following the initial patient call in and screening. This number is referred to as the yield loss (the number of patients who have "dropped out of the surgical process. There are now fewer patients to whom ClearEyes staff will mail paperwork and call to remind to keep their Intake appointments. Another way of looking at this is that we now have fewer patients whom we can bilt; expected revenue will fall! I will walk you through filling in the answers to the first equation. We know that the yield loss is 3156 (14345-11189) patients. How is that number (3156) determined? Please use numbers in your formula and include the total yield loss at each step trounded). Example: The expected formula for the first yield loss should look like this: 88.**** **- 3.156. Please include the comma in thousands separator position. DO NOT include the siensenter only the number Note that at the third yield loss formula, you will need to determine the yield loss separately for the insured patients and cash patients, which add up to the third yield loss U + M. Adding the two together should equal the yield loss for this step. Please keep the tens decimal point for both ) and M. After you add them together, please round to a whole number and you will get the correct yield loss for this step. TASK DETERMINING YIELD LOST THE FORMULA THAT DETERMINES HOW MANY POTENTIAL PATIENTS ARE LOST AFTER THE PRECEDING STEP ANNUAL DEMAND PROVIDED BY INSTRUCTOR 14,345 Initial patient call 22% defect after this point FORMULA: AXBX-C Mallpaperwork 11.189 X Call to remind 11.189 Round formula answer to whole number Check: A-C-11.189 28% no-show after this point FORMULA: DXEXF Check in at clinic X 8,056 Intake 8.056 Round formula answer to whole number Check: D-F-8,056 intake 8.056 Round formula answer to whole number Check: D-F-8,056 74% insured, 26% cash 30% of insured no-show, 47% of cash # Insured Lost: INSURED LOST FORMULA: (G X HXIX 1%- %) Round formula answer to tens decimal point Check in at clinic 5.283 # Cash Lost: CASH LOST FORMULA: GXKX)XLX -M X %) Round formula answer to tens decimal point Check G-UM] - 5.283 Round U.M to whole number 5.283 Surgery, cleanup, record (Staff surgeon 4,611: Connors 672 opsl First next day follow-up 21% no-show after first follow-up FROM CASE 5,283 FORMULA NXOX-P 3-week follow-up 4,174 Round P to whole number Check NP-4.174 1 pts Question 2 What is the patient yield from initial inquiries through surgery? HINT: What percent of the patients who called with initial inquiries had operations? Please round your response to one decimal point. O 29.0% 0 36.8% O 47.2% 65.6% Question 3 1 pts Thinking about the patient yield noted in the previous question, which of the following best reflects your thoughts about the extent of the yield loss from initial inquiries through surgery? We are keeping busy o We could do better We have work to do o We are losing too many of our potential patients Question 4 1 pts Which of the following true statement BEST states why it is important to understand what is driving the operation yield loss for the ClearEyes Clinic? Operations are the clinic core business The clinic is experiencing an unacceptable yield loss O Increased revenue is based on increasing the number of potential patients continuing through to the operation stage Next steps for this clinic will depend on decisions about increasing patient throughout 1 pts Question 5 How many yield loss points occur prior to surgery? 01 O2 03 04 1 pts Question 6 What is the patient yield loss following the initial Patient Call? Note: How many of the initial callers are screened out by PSRs who take the call? Question 7 1 pts What is the patient yield loss prior to the patient checking in for his/her intake appointment? Note: How many of the patients accepted by ClearEyes do not return for an intake appointment? Question 8 1 pts What is the patient yield loss following intake? Note: How many of the patients who completed their intake appointment do not return for their scheduled surgery? Question 9 1 pts Question 9 By what percent would OR patient volume change if ClearEyes cut in half the number of patients who complete intake but fail to show up for surgery? HINT: OR patient volume would increase by 1/2 of the number of patients currently being lost after intake and before checking in for their operation. Determine that number. Divide that number by the number of patients who previously checked in at the clinic for their operation. Note: Keep one decimal point for the new number of patients having surgery. Question 10 1 pts What is the patient yield loss for the ClearEyes Clinic from patient call in to surgery? HINT: How many patients are lost to the clinic between initial contact and surgery? Question 11 1 pts How many patients are lost after their first follow-up appointment? Note: How many patients who have had their operation fail to return for their second follow-up appointment to checkup on the progress of their healing and vision three weeks after surgery? => It is important to note the following: (a) we can assume that these patients have no complaints (though it is possible that some are upset and so refuse to return), and (b) their not returning has no effect on revenue (as the charge for follow-up visits is included in the operation charge) 1 pts Question 12 At which point does the clinic lose the greatest percent of patients? Following the initial call O Patients who do not show up for their Intake Appointment O Patients who do not return for their scheduled surgery Patients who do not return for their second post-op visit 1 pts Question 13 This question summarizes ClearEyes Cataracts Clinic's yield loss. % The final 5,283 operations result from 14,345 initial inquiries, for a yield of What percent of the initial contacts are not getting their operations at ClearEyes? % Please round your numbers and enter a number with one decimal point. The percent sign is not needed. BRIEF CASES 9-916-503 JANUARY 15, 2016 ROY SHAPIRO PAUL MORRISON ClearEyes Cataracts Clinic In the fall of 2015, Dr. Julia Connors was thinking about whether to expand her business, ClearEyes Cataracts Clinic, and, if so, how. After some consideration, Connors decided to share some of her ideas with Nieves Morales, one of her best employees and one whose judgment she trusted. She received this response from Morales: "Dr. Connors, I do not believe that will work. Expanding the clinic that way, with extra hours and more days for all of us, will just make a huge problem. I really think that all the good we have accomplished here will be in serious danger. With that, Morales turned and walked away. Connors stood near the reception desk of her clinic Skeling surprised, puzzled, and worried. Connors had founded the Boston-area clinic in 2012 in the predominantly Latino neighborhood of East Boston and had been the CEO and sole proprietor ever since. Creating, owning, and running her own company had fulfilled a lifelong ambition. By the end of its first year of operations, the clinic was on sound financial footing, and it had become quite profitable since then. Initially, Connors had grown the business by building awareness about cataracts and interest in her clinic through advertising on local radio stations and in free local papers. She did not believe that most of her target audience used the Internet very often, and considered television advertising too expensive. Her own advertising strategy, plus word of mouth and referrals by local ophthalmologists, generated about as much demand as she could handle. Connors spent $48,000 on this advertising in 2014, down from $62,000 in 2012. She asked patients how they had heard about ClearEyes, but most of the respondents were either unsure or named multiple sources. In fact, some of these sources were media that Connors had never used, so she stopped trying to collect this information Connors believed that there was an opportunity to grow her company, but did not know to how to do it. Should she expand the number of rooms of her clinic, and if so, by how many? Should she increase the clinic's hours? Should she try some combination of both? It seemed to her that apart from a larger facility or being open for more hours each week, there ought to be a way for her to turn more of the potential patients who called in into actual served patients, which a friend of hers described as HBS Probeer Emer Roy Shapiro and Paul Morrison, msistant professor at Boston University, prepared this coely as a basis for dess discussion and not an endorsement, source of primary data or an illustration of effective or ineffective management. This can be fictition and any emblance to actual persons or entities is coincidental. The authors wish to thank James Bryan, MD, Los Angeles, who provided walence in the preparation of this case Copyright 2016 President and follows of Harvard College. To order copies or permission to reproduce materials call 1.054-7685 wie Harvard Business Publishing Boston, MA 02163. O to http://www.hspharvard.edu. This publication mwy not be sad, photocopied, or herwise reproduced, sted, or transmitted without the permission of Harvard Business School This document is authorized for use only by JOSE QUINTANA in 2020 916-os I Clearlyes Cataracts Clinie a "Yield problem." She had not run the numbers, but she felt that many initial calls and event visits never turned into real work for the clinic. Cataracts and Procedures to Fix Them A cataract is a progressive deterioration in the comeal lens within the eye that makes the normally transparent lens cloudy. If not treated, this condition can lead to blindness, as light entering the eye is blocked from passing through the lens to the retina's light-sensing cells at the back of the eye. Aging is the most common cause of cataracts, it has been estimated that about 50% of the population at 80 years of age would either have some degree of lens cloudiness or had already had surgery. Other risk factors for cataracts included obesity, diabetes, smoking and exposure to ultraviolet rays. There were several ways to carry out the cataract procedure, but the most common one used in 2015 was phacoemulsification (phaco). In this procedure, the doctor makes a tiny incision in the eye and inserts a small wand. The tip of this wand breaks up the cloudy lens into tiny pieces, using ultrasound, and then vacuums out the pieces. An artificial monofocal intraocular lens (IOL) is folded up, inserted through the incision, and unfolded into position. The procedure can also be used to insert a lens to correct astigmatism. Typically, no sutures are needed to close the tiny incision, and the entire operation takes 10 to 15 minutes. Local anesthesia numbs the eye, and patients receive a mild hypnotic to help them relax and stay still. There is no need for elaborate preoperative preparation Patients can go home after the operation, but are not allowed to drive immediately afterward. Most people experience some degree of improved eyesight immediately. This improvement continues until the eye is fully healed, usually within a month. Although many patients have cataracts in both eyes, they are advised to treat only one eye at a time. The Cataract Surgery Market In 2014, approximately three million cataract operations were performed in the United States. Although new equipment and techniques were constantly being developed and tested, cataract surgery was a straightforward, fairly mature procedure with a low rate of failure and medical complications There was considerable competition for cataract patients because the procedure had many attractive characteristics to the provider organizations. First, it was recognized as a "medical necessity" and was therefore reimbursed by Medicare and by medical insurance companies, although some people paid for the procedure as an out-of-pocket expense. In 2013, prices for most monofocal IOL procedures ranged from $1,500 to $3,500, the average price was about $2,188. The diagnosis of cataracts was relatively quick and easy, and misdiagnosis was rare. The surgery was done on an outpatient basis. Compared with many other specialized medical offices, cataract clinics were relatively simple operations to maintain: Facilities that supported extensive patient care before or after the procedure were not needed, the operating room needed only inexpensive equipment, and malpractice insurance was relatively low because there were rarely complications or failures. Connors believed that there were several reasons that the market for cataract surgery would continue to grow strongly. First, baby boomers, who were born between 1946 and 1964, were becoming senior citizens, and cataracts were attributable primarily to aging. Second, immigration to the United States continued to bring millions of people into the American health care system. Many Marilyn Haddrill, "Cataract Surgery Cost," www.allaboutvision.com/conditions/cataract-surgery.co.thom, December 22. 2015, accessed January 25, 2016. 2 BRIEFCASES I HARVARD BUSINESS SCHOOL This documents whored for use only by JOSE QUINTANA in 2020 Clearlyes Cataracts Clinic 1916- immigrants had worked for years without eye protection in extremely bright sunlight, whose ultraviolet rays could lead to cataract damage. Second, cataract surgery was inexpensive enough that many people might pay for it out of pocket even if they were uninsured. Third, the 2010 passage of the Patient Protection and Affordable Care Act (also known as Obamacare) had expanded access to health insurance for millions of previously uninsured Americans, some of whom would seek this procedure to improve their vision. Fourth, obesity and diabetes, which increased the risk of developing cataracts, continued to afflict many people, and the incidence of these conditions was known to increase with age. Smoking another factor that led to the formation of cataracts, was decreasing, but remained high among some population segments, including many who had obtained health insurance for the first time. Procedures at ClearEyes Cataracts Clinic Connors had gathered detailed information about her company's operations in order to weigh the merits of different expansion paths. The following description summarizes her data. In 2014, ClearEyes carried out 5,283 procedures, for which it received an average payment of $1,338. It operated five days a week, 48 weeks a year, from 9 a.m. to 6 p.m. Connors tracked local competition closely and adjusted her prices as necessary, in order to be the preferred low-cost provider. ClearEyes was closed on Sundays and Mondays, although a single technician came in on Sundays to preform postoperative checkups. All staff other than the staff surgeon had a half-hour lunch and two 15-minute breaks during the day, the surgeon's lunch and breaks totaled two hours. The total non-staff, direct variable cost (primarily medical supplies, including the IOL lens) averaged $480 per operan The clinic owned a 4,100-square-foot building in East Boston. The mortgage, taxes, and utilities on the building cost $5,000 per month. The clinic used 60% of the space and rented the rest to a small company for $2,000 per month. Connors believed that she could end the tenant's lease and expand into the additional space, if she wished, with three months' notice and a one-time payment of about $60,000 The clinic's ground floor held a 600-square-foot waiting area with 40 seats (each seat taking up about nine square feet and equipped with an 8" 10" screen for individual viewing), a receptionist area, and two private intake rooms (each 10' x 10) where patients, friends, and family members could sit with a patient services representative (PSR) who helped them complete medical and insurance forms. While waiting patients were asked to watch videos about cataracts and stylized depictions of the procedure and postoperative care. The screens also offered 40 cable channels. See Exhibit 1 for the clinic layout Patients typically called the clinic after they had been referred by an ophthalmologist or another doctor who believed that the patient had cataracts, or when the patient concluded on his or her own that they might have cataracts. Over the phone, one of the four PSRS took about seven minutes to get patient information, enter into the records system, and schedule an intake appointment for paperwork and payment (see below). PSRs were bilingual in English and Spanish, and one also spoke Portuguese. The PSR asked some questions to try to make certain that the caller had cataracts and to try to screen out patients with complicating medical conditions. About 22% of all callers were screened out due to such conditions or, much less often, for presenting no evidence of cataracts. See Exhibit 2 for a list of tasks and task-times by type of employee If an ophthalmologist had referred the patient, that doctor would already have measured the patient for the new, artificial lens. If the patient had not seen a doctor or been measured for a new HARVARD BUSINESS SCHOOL I BRIEFCASES This document is there for only by JOSE QUINTANA in 2020 After brainstorming with her staff, Connors and her staff jointly developed, tested, and refined a set of questions during the reminder conversation designed to determine the probability that a patient would appear on the day of surgery. Over time, her staff had learned to listen carefully and then shrewdly score each conversation as good, probable, or weak. The clinic overscheduled to compensate for each day's mix of probable and weak appointments. The procedure was working effectively enough so that the staff surgeon and Connors, who also operated as needed, was rarely idle; patients seldom waited more than an hour beyond their scheduled arrival time. The PSRs and the receptionist had stocks of We're so sorry! baskets of wine, gourmet coffee, and chocolate, which they handed out to patients who were thus delayed. Connors felt that her PSRS varied in their ability to get patients to attend intake appointments and then to arrive subsequently for surgery. She had also noticed that some of them "went off script," but was not sure this was a bad thing as the most common "offender" was Gabriela Herrera, who seemed to have more patients showing up than anyone else did despite working the same number of hours. Connors also believed that some PSRs asked more questions than did others. Because all calls and intake interviews recorded which PSR attended to these tasks, Connors discovered that rates of no- show patients differed by PSR, as shown in Exhibit 3c. She wondered what Gabriela was doing better. The actual medical procedure began when one of three technicians brought a patient to one of three surgery rooms, where the patient was "prepped" for surgery. This took 10 minutes, on average. The staff surgeon (or Connors, who operated 672 times in 2013) would enter, introduce herself, and carry out the operation. After she was done, she was able to tell virtually all of the patients that everything was looking good. She would then proceed to the next patient. The surgeon's time in the room averaged 12 minutes, but the clinic scheduled 15. Once out of the room, the surgeon took an additional five minutes to change gowns, wash up, and record the surgery. The technician applied eye bandaging and walked the patient back to the waiting area, which took five minutes. Between surgeries, a cleaning employee took three minutes to prepare the rooms for the next medical use. It also took three minutes to prepare between follow-up visits in the examining rooms, as indicated in Exhibit 2. See Exhibit 4 for a representative two-hour block of scheduling. If the technician judged that the patient was feeling well or calm, she seated the patient in the waiting room among others who were awaiting surgery. If the patient seemed distressed or disgruntled in any way, the patient and anyone with them were seated in another area. Patients and any friends or family members with them were asked to wait for 30 minutes, after which they were allowed to leave after a PSR helped them to sign the paperwork indicating that the operation was complete, schedule the patient's return the next day, and remind them of the steps for postoperative care. This took about four minutes. The next day, patients returned for a checkup on the progress of the healing, which took one minute of conferring with the receptionist. It then took a technician ten minutes, on average, to walk the patient to one of two examining rooms, check the eye, clean or bandage it as necessary, walk them back to the receptionist, and schedule the next follow-up appointment. The examining rooms were also cleaned for three minutes following the checkup. For surgeries that took place on Saturdays, a single technician handled these tasks (checkup and cleaning) on Sundays. Three weeks after the operation, a technician repeated this process in eight minutes (without any need to schedule another visit). About 21% of patients did not return for the three-week check. In rare cases patients called afterward, complaining about some aspect of healing or their vision. In these instances, ClearEyes asked them to come in to see what problem there might be, if any. HARVARD BUSINESS SCHOOL I BRIEFCASES 916-503 1 ClearEyes Cataracts Clinic Exhibit 2 ClearEyes Process Flow, Demand, Capacity, Utilization PSR Minutes Demand Receptionist 7 14.15 Technician Staff Surg Cleaner 100,415 1 Task, Annual Demand, and Job Titles Initial patient call 22 defect after this point Mail paperwork Call to remind 40% reschedule call 28% no-show after this point Check in at dink 11.189 11189 4426 11,199 22.373 2 2 16112 2 20 8.056 161120 8.056 2 2 16.112 6.444 10566 2 10 20 5.280 5.23 5.23 S2830 92.220 74% insured, 26% cash Reminder call 40% reschedule call 30% of insured no-show, 47% of cash check in at dink Prep for surgery Surgery, Cleanup. Record (Staff surgeon 4,611,Connors 672 ops) Bandage, walk to waiting Room cleaning PSR checks patient out First next day) follow-up Tuesday-Saturday room clean (OS) Sunday room clean (20%) 3-week follow-up 21% no-show her first follow-up 3-weekroom dan 26.415 15.849 5 3 4 10 3 3 8 520 5.23 5.20 5.233 21.132 52.330 12.678 1,057 4.174 3.171 32 3 4174 Total anual minutes tunk time/job title: workers by job title 26,678 1 070 16 3 13.440 1 1 41,049 1 2 Intake room 2 Examining rooms 3 Surgical rooms Staff surgeon completes (5,20 - 672) = 4,611 operations per year; Connons completes 672 10 BRIEFCASES I HARVARD BUSINESS SCHOOL brony JOSE QUINTANA Background In the ClearEyes Cataracts Clinic Case, we are told that Dr. Julia Connors has a busy, financially successful cataract clinic and that she wishes to expand to take advantage of unmet demand. She is considering four expansion alternatives: First, she could keep her physical facility as is and extend the hours. Second, she might expand space in the same building that she currently owns, with additional equipment and fixtures within her building. The third option is to expand at a new location. A fourth alternative, which is the focus of the case analysis, would increase volume by increasing the yield of potential patients, most of whom currently drop out before completing the process. An important problem in health care operations involves yield management in health clinics where patients often "drop out" and do not arrive for scheduled appointments (are "no-shows"). It is important to understand the dynamics of this decrease in patient yield if we are going to take action to improve the yield. Instruction Familiarity with the general content of the ClearEyes Cataracts Clinic Case will prepare you to complete this assignment. If you have not done so already, please read pages 1-5 of the case and become familiar with Exhibit 2 on page 10. The case is available HERE. You will concentrate your efforts on Exhibit 2 for this assignment. It is important that you realize on what the annual demand numbers (found in the third column) are based and what causes them to decrease over time (the decreasing patient yield). We will use these annual demand numbers to look at capacity utilization in future assignments and make decisions on how patient volume, capacity utilization, and financial outcomes change in response to proposed changes in the process. Please answer the following questions as specifically as you can. 34 pts Question 1 Below is a matrix containing Information taken directly from Exhibit2 of the ClearEyes Case. Note that not all the information from Exhibit 2 is included. We are specifically interested in examining the decreasing patient yield. We want to know why the clinic is losing patients the further they advance in the process. For this first question, please enter the numbers that complete the formula you would use to determine the viel loss the number of patients lost at each step in the process where the annual demand decreases to answer the first formula (AXBX-Cl. you will have to enter three numbers A, B, and in the empty boxes following the formula. This formula will give you the number of patients lost to ClearEyes following the initial patient call in and screening. This number is referred to as the yield loss (the number of patients who have "dropped out of the surgical process. There are now fewer patients to whom ClearEyes staff will mail paperwork and call to remind to keep their Intake appointments. Another way of looking at this is that we now have fewer patients whom we can bilt; expected revenue will fall! I will walk you through filling in the answers to the first equation. We know that the yield loss is 3156 (14345-11189) patients. How is that number (3156) determined? Please use numbers in your formula and include the total yield loss at each step trounded). Example: The expected formula for the first yield loss should look like this: 88.**** **- 3.156. Please include the comma in thousands separator position. DO NOT include the siensenter only the number Note that at the third yield loss formula, you will need to determine the yield loss separately for the insured patients and cash patients, which add up to the third yield loss U + M. Adding the two together should equal the yield loss for this step. Please keep the tens decimal point for both ) and M. After you add them together, please round to a whole number and you will get the correct yield loss for this step. TASK DETERMINING YIELD LOST THE FORMULA THAT DETERMINES HOW MANY POTENTIAL PATIENTS ARE LOST AFTER THE PRECEDING STEP ANNUAL DEMAND PROVIDED BY INSTRUCTOR 14,345 Initial patient call 22% defect after this point FORMULA: AXBX-C Mallpaperwork 11.189 X Call to remind 11.189 Round formula answer to whole number Check: A-C-11.189 28% no-show after this point FORMULA: DXEXF Check in at clinic X 8,056 Intake 8.056 Round formula answer to whole number Check: D-F-8,056 intake 8.056 Round formula answer to whole number Check: D-F-8,056 74% insured, 26% cash 30% of insured no-show, 47% of cash # Insured Lost: INSURED LOST FORMULA: (G X HXIX 1%- %) Round formula answer to tens decimal point Check in at clinic 5.283 # Cash Lost: CASH LOST FORMULA: GXKX)XLX -M X %) Round formula answer to tens decimal point Check G-UM] - 5.283 Round U.M to whole number 5.283 Surgery, cleanup, record (Staff surgeon 4,611: Connors 672 opsl First next day follow-up 21% no-show after first follow-up FROM CASE 5,283 FORMULA NXOX-P 3-week follow-up 4,174 Round P to whole number Check NP-4.174 1 pts Question 2 What is the patient yield from initial inquiries through surgery? HINT: What percent of the patients who called with initial inquiries had operations? Please round your response to one decimal point. O 29.0% 0 36.8% O 47.2% 65.6% Question 3 1 pts Thinking about the patient yield noted in the previous question, which of the following best reflects your thoughts about the extent of the yield loss from initial inquiries through surgery? We are keeping busy o We could do better We have work to do o We are losing too many of our potential patients Question 4 1 pts Which of the following true statement BEST states why it is important to understand what is driving the operation yield loss for the ClearEyes Clinic? Operations are the clinic core business The clinic is experiencing an unacceptable yield loss O Increased revenue is based on increasing the number of potential patients continuing through to the operation stage Next steps for this clinic will depend on decisions about increasing patient throughout 1 pts Question 5 How many yield loss points occur prior to surgery? 01 O2 03 04 1 pts Question 6 What is the patient yield loss following the initial Patient Call? Note: How many of the initial callers are screened out by PSRs who take the call? Question 7 1 pts What is the patient yield loss prior to the patient checking in for his/her intake appointment? Note: How many of the patients accepted by ClearEyes do not return for an intake appointment? Question 8 1 pts What is the patient yield loss following intake? Note: How many of the patients who completed their intake appointment do not return for their scheduled surgery? Question 9 1 pts Question 9 By what percent would OR patient volume change if ClearEyes cut in half the number of patients who complete intake but fail to show up for surgery? HINT: OR patient volume would increase by 1/2 of the number of patients currently being lost after intake and before checking in for their operation. Determine that number. Divide that number by the number of patients who previously checked in at the clinic for their operation. Note: Keep one decimal point for the new number of patients having surgery. Question 10 1 pts What is the patient yield loss for the ClearEyes Clinic from patient call in to surgery? HINT: How many patients are lost to the clinic between initial contact and surgery? Question 11 1 pts How many patients are lost after their first follow-up appointment? Note: How many patients who have had their operation fail to return for their second follow-up appointment to checkup on the progress of their healing and vision three weeks after surgery? => It is important to note the following: (a) we can assume that these patients have no complaints (though it is possible that some are upset and so refuse to return), and (b) their not returning has no effect on revenue (as the charge for follow-up visits is included in the operation charge) 1 pts Question 12 At which point does the clinic lose the greatest percent of patients? Following the initial call O Patients who do not show up for their Intake Appointment O Patients who do not return for their scheduled surgery Patients who do not return for their second post-op visit 1 pts Question 13 This question summarizes ClearEyes Cataracts Clinic's yield loss. % The final 5,283 operations result from 14,345 initial inquiries, for a yield of What percent of the initial contacts are not getting their operations at ClearEyes? % Please round your numbers and enter a number with one decimal point. The percent sign is not needed. BRIEF CASES 9-916-503 JANUARY 15, 2016 ROY SHAPIRO PAUL MORRISON ClearEyes Cataracts Clinic In the fall of 2015, Dr. Julia Connors was thinking about whether to expand her business, ClearEyes Cataracts Clinic, and, if so, how. After some consideration, Connors decided to share some of her ideas with Nieves Morales, one of her best employees and one whose judgment she trusted. She received this response from Morales: "Dr. Connors, I do not believe that will work. Expanding the clinic that way, with extra hours and more days for all of us, will just make a huge problem. I really think that all the good we have accomplished here will be in serious danger. With that, Morales turned and walked away. Connors stood near the reception desk of her clinic Skeling surprised, puzzled, and worried. Connors had founded the Boston-area clinic in 2012 in the predominantly Latino neighborhood of East Boston and had been the CEO and sole proprietor ever since. Creating, owning, and running her own company had fulfilled a lifelong ambition. By the end of its first year of operations, the clinic was on sound financial footing, and it had become quite profitable since then. Initially, Connors had grown the business by building awareness about cataracts and interest in her clinic through advertising on local radio stations and in free local papers. She did not believe that most of her target audience used the Internet very often, and considered television advertising too expensive. Her own advertising strategy, plus word of mouth and referrals by local ophthalmologists, generated about as much demand as she could handle. Connors spent $48,000 on this advertising in 2014, down from $62,000 in 2012. She asked patients how they had heard about ClearEyes, but most of the respondents were either unsure or named multiple sources. In fact, some of these sources were media that Connors had never used, so she stopped trying to collect this information Connors believed that there was an opportunity to grow her company, but did not know to how to do it. Should she expand the number of rooms of her clinic, and if so, by how many? Should she increase the clinic's hours? Should she try some combination of both? It seemed to her that apart from a larger facility or being open for more hours each week, there ought to be a way for her to turn more of the potential patients who called in into actual served patients, which a friend of hers described as HBS Probeer Emer Roy Shapiro and Paul Morrison, msistant professor at Boston University, prepared this coely as a basis for dess discussion and not an endorsement, source of primary data or an illustration of effective or ineffective management. This can be fictition and any emblance to actual persons or entities is coincidental. The authors wish to thank James Bryan, MD, Los Angeles, who provided walence in the preparation of this case Copyright 2016 President and follows of Harvard College. To order copies or permission to reproduce materials call 1.054-7685 wie Harvard Business Publishing Boston, MA 02163. O to http://www.hspharvard.edu. This publication mwy not be sad, photocopied, or herwise reproduced, sted, or transmitted without the permission of Harvard Business School This document is authorized for use only by JOSE QUINTANA in 2020 916-os I Clearlyes Cataracts Clinie a "Yield problem." She had not run the numbers, but she felt that many initial calls and event visits never turned into real work for the clinic. Cataracts and Procedures to Fix Them A cataract is a progressive deterioration in the comeal lens within the eye that makes the normally transparent lens cloudy. If not treated, this condition can lead to blindness, as light entering the eye is blocked from passing through the lens to the retina's light-sensing cells at the back of the eye. Aging is the most common cause of cataracts, it has been estimated that about 50% of the population at 80 years of age would either have some degree of lens cloudiness or had already had surgery. Other risk factors for cataracts included obesity, diabetes, smoking and exposure to ultraviolet rays. There were several ways to carry out the cataract procedure, but the most common one used in 2015 was phacoemulsification (phaco). In this procedure, the doctor makes a tiny incision in the eye and inserts a small wand. The tip of this wand breaks up the cloudy lens into tiny pieces, using ultrasound, and then vacuums out the pieces. An artificial monofocal intraocular lens (IOL) is folded up, inserted through the incision, and unfolded into position. The procedure can also be used to insert a lens to correct astigmatism. Typically, no sutures are needed to close the tiny incision, and the entire operation takes 10 to 15 minutes. Local anesthesia numbs the eye, and patients receive a mild hypnotic to help them relax and stay still. There is no need for elaborate preoperative preparation Patients can go home after the operation, but are not allowed to drive immediately afterward. Most people experience some degree of improved eyesight immediately. This improvement continues until the eye is fully healed, usually within a month. Although many patients have cataracts in both eyes, they are advised to treat only one eye at a time. The Cataract Surgery Market In 2014, approximately three million cataract operations were performed in the United States. Although new equipment and techniques were constantly being developed and tested, cataract surgery was a straightforward, fairly mature procedure with a low rate of failure and medical complications There was considerable competition for cataract patients because the procedure had many attractive characteristics to the provider organizations. First, it was recognized as a "medical necessity" and was therefore reimbursed by Medicare and by medical insurance companies, although some people paid for the procedure as an out-of-pocket expense. In 2013, prices for most monofocal IOL procedures ranged from $1,500 to $3,500, the average price was about $2,188. The diagnosis of cataracts was relatively quick and easy, and misdiagnosis was rare. The surgery was done on an outpatient basis. Compared with many other specialized medical offices, cataract clinics were relatively simple operations to maintain: Facilities that supported extensive patient care before or after the procedure were not needed, the operating room needed only inexpensive equipment, and malpractice insurance was relatively low because there were rarely complications or failures. Connors believed that there were several reasons that the market for cataract surgery would continue to grow strongly. First, baby boomers, who were born between 1946 and 1964, were becoming senior citizens, and cataracts were attributable primarily to aging. Second, immigration to the United States continued to bring millions of people into the American health care system. Many Marilyn Haddrill, "Cataract Surgery Cost," www.allaboutvision.com/conditions/cataract-surgery.co.thom, December 22. 2015, accessed January 25, 2016. 2 BRIEFCASES I HARVARD BUSINESS SCHOOL This documents whored for use only by JOSE QUINTANA in 2020 Clearlyes Cataracts Clinic 1916- immigrants had worked for years without eye protection in extremely bright sunlight, whose ultraviolet rays could lead to cataract damage. Second, cataract surgery was inexpensive enough that many people might pay for it out of pocket even if they were uninsured. Third, the 2010 passage of the Patient Protection and Affordable Care Act (also known as Obamacare) had expanded access to health insurance for millions of previously uninsured Americans, some of whom would seek this procedure to improve their vision. Fourth, obesity and diabetes, which increased the risk of developing cataracts, continued to afflict many people, and the incidence of these conditions was known to increase with age. Smoking another factor that led to the formation of cataracts, was decreasing, but remained high among some population segments, including many who had obtained health insurance for the first time. Procedures at ClearEyes Cataracts Clinic Connors had gathered detailed information about her company's operations in order to weigh the merits of different expansion paths. The following description summarizes her data. In 2014, ClearEyes carried out 5,283 procedures, for which it received an average payment of $1,338. It operated five days a week, 48 weeks a year, from 9 a.m. to 6 p.m. Connors tracked local competition closely and adjusted her prices as necessary, in order to be the preferred low-cost provider. ClearEyes was closed on Sundays and Mondays, although a single technician came in on Sundays to preform postoperative checkups. All staff other than the staff surgeon had a half-hour lunch and two 15-minute breaks during the day, the surgeon's lunch and breaks totaled two hours. The total non-staff, direct variable cost (primarily medical supplies, including the IOL lens) averaged $480 per operan The clinic owned a 4,100-square-foot building in East Boston. The mortgage, taxes, and utilities on the building cost $5,000 per month. The clinic used 60% of the space and rented the rest to a small company for $2,000 per month. Connors believed that she could end the tenant's lease and expand into the additional space, if she wished, with three months' notice and a one-time payment of about $60,000 The clinic's ground floor held a 600-square-foot waiting area with 40 seats (each seat taking up about nine square feet and equipped with an 8" 10" screen for individual viewing), a receptionist area, and two private intake rooms (each 10' x 10) where patients, friends, and family members could sit with a patient services representative (PSR) who helped them complete medical and insurance forms. While waiting patients were asked to watch videos about cataracts and stylized depictions of the procedure and postoperative care. The screens also offered 40 cable channels. See Exhibit 1 for the clinic layout Patients typically called the clinic after they had been referred by an ophthalmologist or another doctor who believed that the patient had cataracts, or when the patient concluded on his or her own that they might have cataracts. Over the phone, one of the four PSRS took about seven minutes to get patient information, enter into the records system, and schedule an intake appointment for paperwork and payment (see below). PSRs were bilingual in English and Spanish, and one also spoke Portuguese. The PSR asked some questions to try to make certain that the caller had cataracts and to try to screen out patients with complicating medical conditions. About 22% of all callers were screened out due to such conditions or, much less often, for presenting no evidence of cataracts. See Exhibit 2 for a list of tasks and task-times by type of employee If an ophthalmologist had referred the patient, that doctor would already have measured the patient for the new, artificial lens. If the patient had not seen a doctor or been measured for a new HARVARD BUSINESS SCHOOL I BRIEFCASES This document is there for only by JOSE QUINTANA in 2020 After brainstorming with her staff, Connors and her staff jointly developed, tested, and refined a set of questions during the reminder conversation designed to determine the probability that a patient would appear on the day of surgery. Over time, her staff had learned to listen carefully and then shrewdly score each conversation as good, probable, or weak. The clinic overscheduled to compensate for each day's mix of probable and weak appointments. The procedure was working effectively enough so that the staff surgeon and Connors, who also operated as needed, was rarely idle; patients seldom waited more than an hour beyond their scheduled arrival time. The PSRs and the receptionist had stocks of We're so sorry! baskets of wine, gourmet coffee, and chocolate, which they handed out to patients who were thus delayed. Connors felt that her PSRS varied in their ability to get patients to attend intake appointments and then to arrive subsequently for surgery. She had also noticed that some of them "went off script," but was not sure this was a bad thing as the most common "offender" was Gabriela Herrera, who seemed to have more patients showing up than anyone else did despite working the same number of hours. Connors also believed that some PSRs asked more questions than did others. Because all calls and intake interviews recorded which PSR attended to these tasks, Connors discovered that rates of no- show patients differed by PSR, as shown in Exhibit 3c. She wondered what Gabriela was doing better. The actual medical procedure began when one of three technicians brought a patient to one of three surgery rooms, where the patient was "prepped" for surgery. This took 10 minutes, on average. The staff surgeon (or Connors, who operated 672 times in 2013) would enter, introduce herself, and carry out the operation. After she was done, she was able to tell virtually all of the patients that everything was looking good. She would then proceed to the next patient. The surgeon's time in the room averaged 12 minutes, but the clinic scheduled 15. Once out of the room, the surgeon took an additional five minutes to change gowns, wash up, and record the surgery. The technician applied eye bandaging and walked the patient back to the waiting area, which took five minutes. Between surgeries, a cleaning employee took three minutes to prepare the rooms for the next medical use. It also took three minutes to prepare between follow-up visits in the examining rooms, as indicated in Exhibit 2. See Exhibit 4 for a representative two-hour block of scheduling. If the technician judged that the patient was feeling well or calm, she seated the patient in the waiting room among others who were awaiting surgery. If the patient seemed distressed or disgruntled in any way, the patient and anyone with them were seated in another area. Patients and any friends or family members with them were asked to wait for 30 minutes, after which they were allowed to leave after a PSR helped them to sign the paperwork indicating that the operation was complete, schedule the patient's return the next day, and remind them of the steps for postoperative care. This took about four minutes. The next day, patients returned for a checkup on the progress of the healing, which took one minute of conferring with the receptionist. It then took a technician ten minutes, on average, to walk the patient to one of two examining rooms, check the eye, clean or bandage it as necessary, walk them back to the receptionist, and schedule the next follow-up appointment. The examining rooms were also cleaned for three minutes following the checkup. For surgeries that took place on Saturdays, a single technician handled these tasks (checkup and cleaning) on Sundays. Three weeks after the operation, a technician repeated this process in eight minutes (without any need to schedule another visit). About 21% of patients did not return for the three-week check. In rare cases patients called afterward, complaining about some aspect of healing or their vision. In these instances, ClearEyes asked them to come in to see what problem there might be, if any. HARVARD BUSINESS SCHOOL I BRIEFCASES 916-503 1 ClearEyes Cataracts Clinic Exhibit 2 ClearEyes Process Flow, Demand, Capacity, Utilization PSR Minutes Demand Receptionist 7 14.15 Technician Staff Surg Cleaner 100,415 1 Task, Annual Demand, and Job Titles Initial patient call 22 defect after this point Mail paperwork Call to remind 40% reschedule call 28% no-show after this point Check in at dink 11.189 11189 4426 11,199 22.373 2 2 16112 2 20 8.056 161120 8.056 2 2 16.112 6.444 10566 2 10 20 5.280 5.23 5.23 S2830 92.220 74% insured, 26% cash Reminder call 40% reschedule call 30% of insured no-show, 47% of cash check in at dink Prep for surgery Surgery, Cleanup. Record (Staff surgeon 4,611,Connors 672 ops) Bandage, walk to waiting Room cleaning PSR checks patient out First next day) follow-up Tuesday-Saturday room clean (OS) Sunday room clean (20%) 3-week follow-up 21% no-show her first follow-up 3-weekroom dan 26.415 15.849 5 3 4 10 3 3 8 520 5.23 5.20 5.233 21.132 52.330 12.678 1,057 4.174 3.171 32 3 4174 Total anual minutes tunk time/job title: workers by job title 26,678 1 070 16 3 13.440 1 1 41,049 1 2 Intake room 2 Examining rooms 3 Surgical rooms Staff surgeon completes (5,20 - 672) = 4,611 operations per year; Connons completes 672 10 BRIEFCASES I HARVARD BUSINESS SCHOOL brony JOSE QUINTANA
Step by Step Solution
There are 3 Steps involved in it
1 Expert Approved Answer
Step: 1 Unlock


Question Has Been Solved by an Expert!
Get step-by-step solutions from verified subject matter experts
Step: 2 Unlock
Step: 3 Unlock


