Question: Official coding guidelines are used to ensure accurate coding practices, and coders find it necessary to consistently refer to them when assigning codes to justify
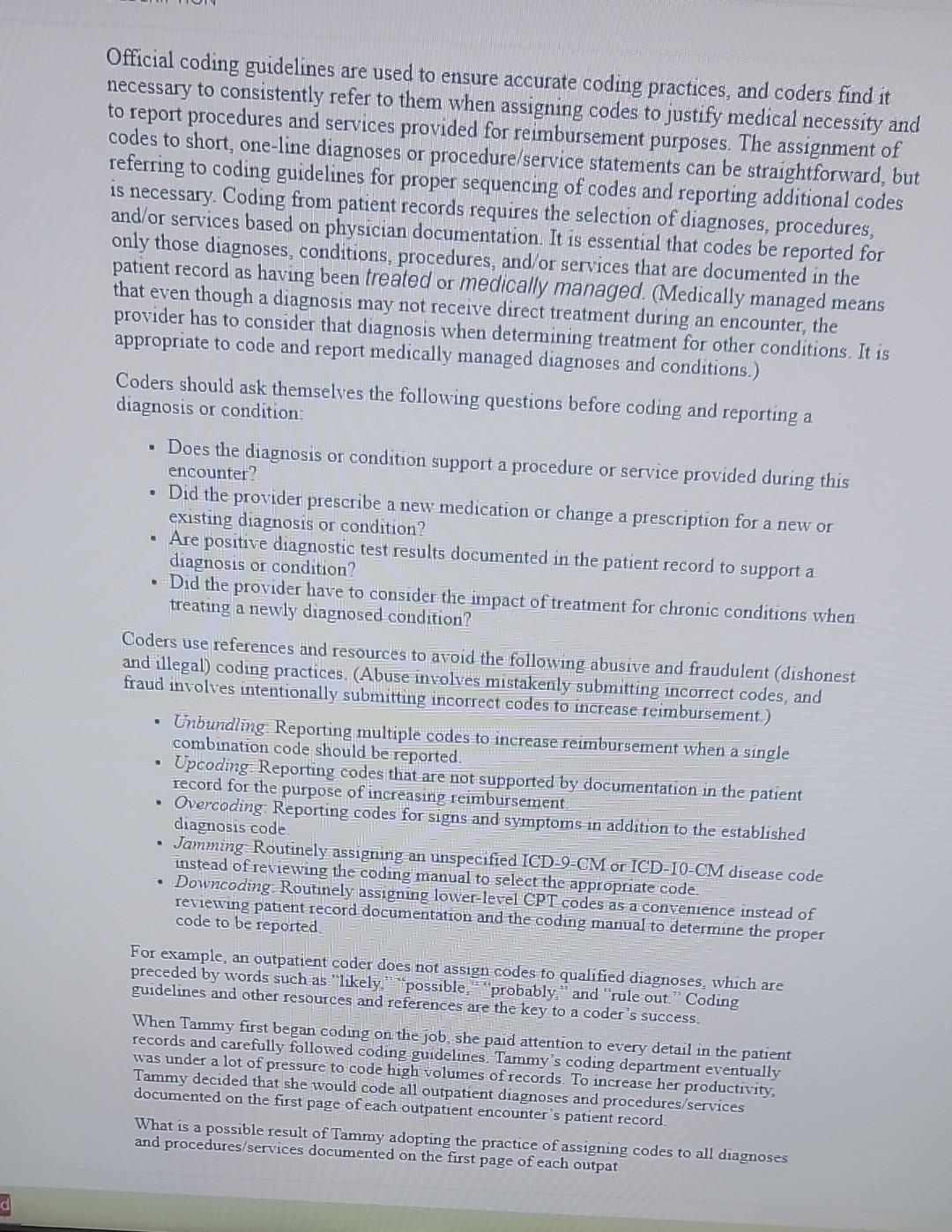
Official coding guidelines are used to ensure accurate coding practices, and coders find it necessary to consistently refer to them when assigning codes to justify medical necessity a to report procedures and services provided for reimbursement purposes. The assignment of codes to short, one-line diagnoses or procedure/service statements can be straightforward, b referring to coding guidelines for proper sequencing of codes and reporting additional codes is necessary. Coding from patient records requires the selection of diagnoses, procedures, and/or services based on physician documentation. It is essential that codes be reported for only those diagnoses, conditions, procedures, and/or services that are documented in the patient record as having been treated or medically managed. (Medically managed means that even though a diagnosis may not receive direct treatment during an encounter, the provider has to consider that diagnosis when determining treatment for other conditions. It is appropriate to code and report medically managed diagnoses and conditions.) Coders should ask themselves the following questions before coding and reporting a diagnosis or condition: - Does the diagnosis or condition support a procedure or service provided during this encounter? - Did the provider prescribe a new medication or change a prescription for a new or existing diagnosis or condition? - Are positive diagnostic test results documented in the patient record to support a diagnosis or condition? - Did the provider have to consider the impact of treatment for chronic conditions when treating a newly diagnosed condition? Coders use references and resources to aroid the following abusive and fraudulent (dishonest and illegal) coding practices. (Abuse involves mistakenly submitting incorrect codes, and fraud involves intentionally submitting incorrect codes to increase reimbursement.) - Unbundlng: Reporting multiple codes to increase reimbursement when a single combination code should be reported. - Upcoding:Reporting codes that are not supported by documentation in the patient record for the purpose of increasing reimbursement - Overcoding: Reporting codes for signs and symptoms in addition to the established diagnosis code. - Jamming Routinely assigning an unspecified ICD-9-CM or ICD-10-CM disease code instead of reviewing the coding manual to seleet the appropriate code. - Downcoding Routinely assigning lower-level CPT codes as a convenience instead of reviewing patient record documentation and the coding manual to determine the proper code to be reported. For example, an outpatient coder does not assign-codes to qualified diagnoses, which are preceded by words such as "likely, "possible, "probably": "and "rule out." Coding guidelines and other resources and references are the key to a coder's success. When Tammy first began coding on the job, she paid attention to every detail in the patient records and carefully followed coding guidelines. Tammy's coding department eventually Tammy decided that she would to code high volumes of records. To increase her productiv documented on the first page of each outpatient encounter's patient record. What is a possible result of Tammy adopting the practice of assigning codes to all diagnoses and procedures/services documented on the first page of each outpat
Step by Step Solution
There are 3 Steps involved in it

Get step-by-step solutions from verified subject matter experts


